A estenose aórtica (EA) é uma doença valvular e vascular sistémica, com elevada prevalência nos países desenvolvidos. A nova entidade «EA grave paradoxal, baixo fluxo/baixo gradiente» refere‐se aos casos em que os doentes apresentam EA grave com base na avaliação da área valvular aórtica (AVA) (≤1cm2) ou AVA indexada (≤0,6cm2/m2), mas que paradoxalmente tenham um gradiente médio transvalvular baixo (<40mmHg), com baixo volume de ejeção sistólico indexado (≤35ml/m2), apesar de uma fração de ejeção do ventrículo esquerdo preservada (≥50%).
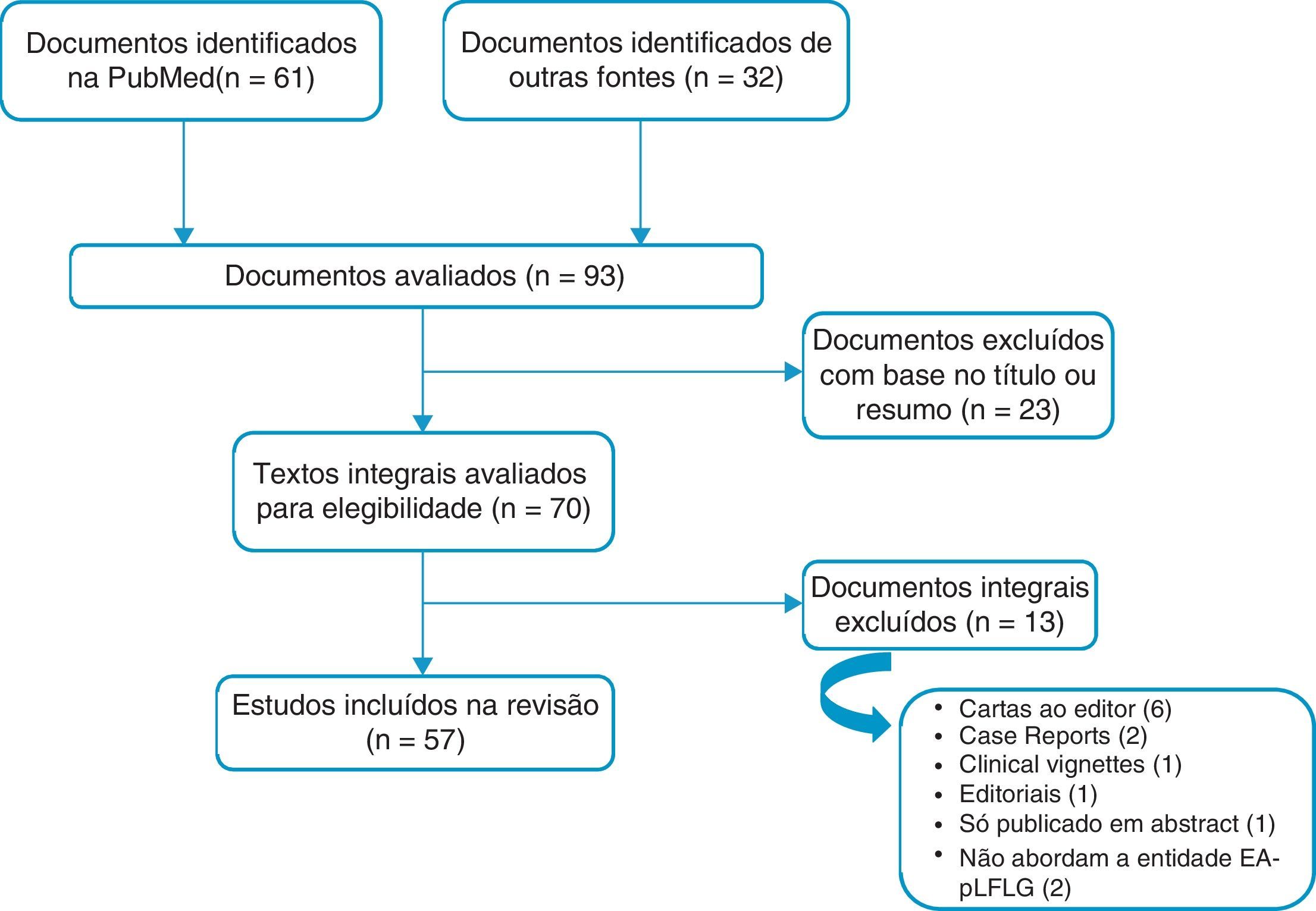
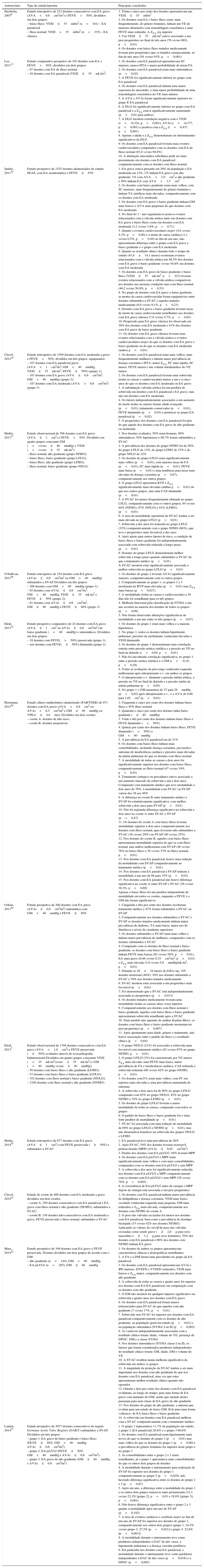
Foi realizada uma pesquisa através da base de dados da PubMed sobre a EA paradoxal no período de 2007‐2014. Para a presente revisão foram incluídos um total de 57 artigos.
A prevalência da EA paradoxal variou entre 3‐35% da população com EA degenerativa grave. Foi mais frequente no género feminino e nos doentes com idade mais avançada, e esteve associada a uma remodelagem característica do ventrículo esquerdo, bem como a um aumento da rigidez vascular arterial sistémica. Assinala‐se a possibilidade de erros e imprecisões no cálculo da AVA pela equação da continuidade, que podem sugerir o fenótipo paradoxal. Existem outros métodos de diagnóstico que podem auxiliar no estudo da EA, como o score de cálcio, a avaliação da impedância valvuloarterial e o estudo da mecânica longitudinal do ventrículo esquerdo. Relativamente à história natural, não é claro que a EA paradoxal corresponda a uma fase avançada da doença valvular aórtica, ou se representa um fenótipo distinto com especificidades próprias. A terapêutica de substituição valvular, cirúrgica ou percutânea, pode estar indicada no doente com EA paradoxal grave e sintomática.
Aortic stenosis (AS) is a complex systemic valvular and vascular disease with a high prevalence in developed countries. The new entity “paradoxical low‐flow, low‐gradient aortic stenosis” refers to cases in which patients have severe AS based on assessment of aortic valve area (AVA) (≤1 cm2) or indexed AVA (≤0.6 cm2/m2), but paradoxically have a low mean transvalvular gradient (<40 mmHg) and a low stroke volume index (≤35 ml/m2), despite preserved left ventricular ejection fraction (≥50%).
A search was carried out in the PubMed database on paradoxical AS for the period 2007‐2014. A total of 57 articles were included for this review. The prevalence of paradoxical AS ranged from 3% to 35% of the population with severe degenerative AS. It was more frequent in females and in older patients. Paradoxical AS was associated with characteristic left ventricular remodeling as well as an increase in systemic arterial stiffness. It was noted that there may be errors and inaccuracies in the calculation of AVA by the continuity equation, which could erroneously suggest the paradoxical phenotype. There are new diagnostic methods to facilitate the study of AS, such as aortic valve calcium score, valvuloarterial impedance and the longitudinal mechanics of the left ventricle. With regard to its natural history, it is not clear whether paradoxical AS corresponds to an advance stage of the disease or if paradoxical AS patients have a distinct phenotype with specific characteristics. Valve replacement, either surgical or percutaneous, may be indicated in patients with severe and symptomatic paradoxical AS.
Área valvular aórtica
Área valvular aórtica indexada
Área valvular aórtica projetada indexada
Brain natriuretic peptide
Compliance arterial sistémica
Doença coronária
Deformação global longitudinal
Estenose aórtica
Estenose aórtica de baixo fluxo e baixo gradiente
Espessura relativa da parede
Fibrilhação auricular
Frequência cardíaca
Fração de ejeção do ventrículo esquerdo
Gradiente médio transvalvular ventrículo esquerdo/aorta
Hipertensão arterial
Índice de perda de energia
Placement of AoRTic TranscathetER Valve Trial Edwards SAPIEN Transcatheter Heart Valve
Ressonância magnética cardíaca
Resistência valvular periférica
Simvastatin and ezetimibe in aortic stenosis
Superfície corporal
Substituição valvular aórtica cirúrgica
Substituição valvular aórtica percutânea
Tensão arterial
Trato de saída do ventrículo esquerdo
Ventrículo esquerdo
Velocidade de pico de ejeção aórtica
Volume ejeção sistólico indexado
Impedância valvuloarterial
A estenose aórtica (EA) é a valvulopatia mais frequente na Europa e a etiologia degenerativa é a mais comum1. Estima‐se que afete 2‐7% da população com mais de 65 anos2. A EA degenerativa tem uma progressão lenta e está associada a diferentes manifestações clínicas como a angina, a síncope, as perturbações do ritmo cardíaco, a insuficiência cardíaca e a morte súbita1.
De acordo com o documento orientador europeu e norte‐americano sobre doença valvular, a EA grave define‐se, na presença de um débito cardíaco normal, por uma área valvular aórtica (AVA) ≤1,0cm2, um gradiente médio (GM) ventrículo esquerdo (VE)/aorta (Ao) (GM)≥40mmHg ou uma velocidade de pico de ejeção aórtica (VPEA)≥4m/s1,3.
Na ausência de tratamento de substituição valvular, a EA evoluiu para uma forma de falência cardíaca, na qual há dilatação e disfunção sistólica do VE. Esta fase está associada a uma diminuição dos gradientes transvalvulares, porque o fluxo sistólico através da válvula aórtica diminui na sequência da redução do desempenho sistólico do VE. Esta condição foi pela primeira vez descrita por Carabello et al. em 19804 e foi denominada EA baixo‐fluxo baixo‐gradiente (EA‐BFBG). É caracterizada por uma AVA ≤1,0cm2 (ou ≤0,6cm2/m2), um GM<40mmHg e uma fração de ejeção do ventrículo esquerdo (FEVE) ≤40%. Os doentes com EA‐BFBG representam apenas 5‐10% dos doentes com EA grave5–7.
Em 2007, Hachicha et al.8 descreveram, pela primeira vez, uma forma de EA com um fluxo sistólico reduzido mas, paradoxalmente, com um bom desempenho sistólico do VE. Esta nova entidade foi denominada EA paradoxical low‐flow low‐gradient – EA paradoxal – e foi definida pelas seguintes características: AVA ≤1,0cm2; GM<40mmHg; volume de ejeção sistólico indexado (VESI)≤35mL/m2, isto apesar da FEVE≥50%3,5,9. Foi demonstrada uma prevalência significativa da EA paradoxal e foi também reconhecido que este fenótipo pode também representar uma forma avançada de EA8,10.
O presente artigo teve como objetivo elaborar uma revisão sistemática da literatura sobre a EA paradoxal. Serão abordados aspetos relacionados com a definição, características clínicas, diagnóstico, prognóstico, história natural e tratamento.
MétodosFoi realizada uma pesquisa através da base de dados PubMed, a última a 29 de dezembro de 2014, com as seguintes palavras‐chave: «paradoxical aortic valve stenosis» e uma das seguintes: «low flow», ou «low gradient», ou «assessment», ou «left ventricular ejection fraction», ou «echocardiography», ou «treatment», ou «prognosis». A pesquisa compreendeu artigos escritos em inglês, publicados desde 2007. Foram incluídos artigos científicos originais, ensaios clínicos, revisões e ensaios em animais.
Ao aplicar os filtros supracitados, resultaram 61 artigos. Destes 23 foram rejeitados com base no título e no resumo, porque não estavam relacionados com o objetivo do trabalho. Foi realizada a leitura completa dos restantes. Relativamente aos 38 artigos resultantes da pesquisa, assinala‐se que 13 não foram utilizados para a bibliografia do presente documento: seis cartas ao editor, dois casos clínicos e uma clinical vignette; um por só ter sido publicado sob a forma de abstract; dois por não se referirem à EA paradoxal após leitura completa do artigo; e um foi considerado um editorial pouco relevante. Por forma a não deixar de parte nenhum artigo fundamental, foi feita uma revisão à bibliografia dos artigos pesquisados e 32 foram adicionados à pesquisa inicial. Foram também consultadas as recomendações da Sociedade Americana de Cardiologia e da Sociedade Europeia de Cardiologia sobre doença valvular. Para a bibliografia final foram utilizados 57 artigos (Figura 1).
Foi avaliada a qualidade dos principais estudos citados no presente documento, e que estão sumariados na Tabela 1. Esta avaliação foi realizada por um elemento externo à equipa de trabalho. Foi utilizada a escala de Effective Public Health Practice Project (EPHPP) – (http://www.ephpp.ca/tools.html).
EA paradoxal e medicina baseada na evidência
| Autores/ano | Tipo de estudo/amostra | Principais conclusões |
|---|---|---|
| Hachicha, 20078 | Estudo retrospetivo de 512 doentes consecutivos com EA grave (AVA<0,6cm2/m2) e FEVE>50%, divididos em dois grupos: – baixo fluxo: VESI≤35ml/m2 (n=181) – EA paradoxal – fluxo normal: VESI>35ml/m2 (n=335) – EA clássica | 1. Trinta e cinco por cento dos doentes apresentavam um VESI≤35ml/m2 2. Os doentes com EA e baixo fluxo eram, mais frequentemente, do género feminino, tinham um VE de menores dimensões com remodelagem concêntrica e uma FEVE mais reduzida. A ZVA era superior 3. Um VESI≤35mL/m2 esteve associado a um pior prognóstico ao final de três anos (76 versus 86%, p<0,01) 4. Os doentes com baixo fluxo tratados medicamente tiveram pior prognóstico que os tratados cirurgicamente, ao fim de três anos (58 versus 93%, p=0,001) |
| Lee, 201113 | Estudo comparativo prospetivo de 103 doentes com EA e FEVE>50%, divididos em dois grupos: – 87 doentes com EA de fluxo normal; – 16 doentes com EA paradoxal (VESI≤35mL/m2) | 1. Os doentes com EA paradoxal apresentavam SC maiores, menos HTA e maior probabilidade de terem FA 2. Os doentes com EA paradoxal eram mais sintomáticos (p=0,02) 3. A FEVE foi significativamente inferior no grupo com EA paradoxal 4. Os doentes com EA paradoxal tinham uma maior espessura do miocárdio, e uma maior probabilidade de uma remodelagem concêntrica do VE mais intensa 5. A AVA e AVAi foram significativamente menores no grupo E EA paradoxal 6. A DLG foi significativamente inferior no grupo com EA paradoxal e a ZVA estava significativamente aumentada (p<0,01 para ambos) 7. A DLG mostrou correlação negativa com o VESI (r=‐0,324, p=0,001), AVAi (r=‐0,377, p<0,001) e positiva com a ZVA (r=0,437, p<0,001) 8. Apenas a idade e a ZVA demonstraram ser determinantes significativos da DLG 9. Os doentes com EA paradoxal tiveram mais eventos cardiovasculares comparados com os doentes com EA de fluxo normal (93,8 versus 69,8%) 10. A disfunção miocárdica subclínica pode ser mais proeminente em doentes com EA paradoxal comparativamente com os doentes com fluxo normal |
| Jander, 201152 | Estudo prospetivo de 1525 doentes aleatorizados do estudo SEAS, com EA assintomática e FEVE≥55% | 1. EA grave estava presente em 29% da população e EA moderada em 12%, 2% tinham EA grave com alto gradiente, 1% com AVA>1,0cm2 e alto gradiente e 56% tinham EA com AVA>1,5cm2 2. Os doentes com baixo gradiente eram mais velhos, com SC menores, mais frequentemente do género feminino e tinham TA sistólicas mais elevadas, comparativamente com os doentes com EA moderada 3. Os doentes com EA grave e baixo gradiente tinham GM mais baixos e AVA mais pequenas do que doentes com EA moderada 4. No final do 1.° ano registaram‐se poucos eventos relacionados com a válvula aórtica tanto em doentes com EA grave e baixo fluxo como em doentes com EA moderada (3,2 versus 3,8%, p=0,71) 5. Quanto a eventos cardiovasculares major (4,8 versus 4,3%, p=0,80) e a morte de causa cardíaca (1,1 versus 0,5%, p=0,49) ao fim de um ano, não apresentaram diferença entre o grupo com EA grave e baixo gradiente e o grupo com EA moderada 6. Quanto ao resultado clínico durante todo o tempo de estudo (45,8±14,1 meses) ocorreram eventos relacionados com a válvula aórtica em 48,5% dos doentes com EA grave e baixo gradiente versus 44,6% em doentes com EA moderada 7. Os doentes com EA grave de baixo gradiente e baixo fluxo (VESI≤35mL/m2, n=223) tiveram eventos relacionados com a válvula aórtica comparáveis aos doentes nas mesmas condições mas com fluxo normal (46,2 versus 50,9%, p=0,53) 8. No grupo de doentes com EA grave e baixo gradiente, as mortes de causa cardiovascular foram equiparáveis entre doentes submetidos a SVAC e aqueles tratados medicamente (6,0 versus 9,1%, p=0,23) 9. Doentes com EA grave e baixo gradiente tiveram taxas de morte de causa cardiovascular semelhantes aos doentes com EA grave clássica (7,8 versus 5,7%, p=0,65) 10. Progressão para EA grave clássica foi observada em 38% dos doentes com EA moderada e 41% dos doentes com EA grave de baixo gradiente 11. Os doentes com EA grave clássica tiveram mais eventos relacionados com a válvula aórtica e eventos cardiovasculares major do que os doentes com EA grave e baixo gradiente ou do que os doentes com EA moderada (ambos p<0,01) |
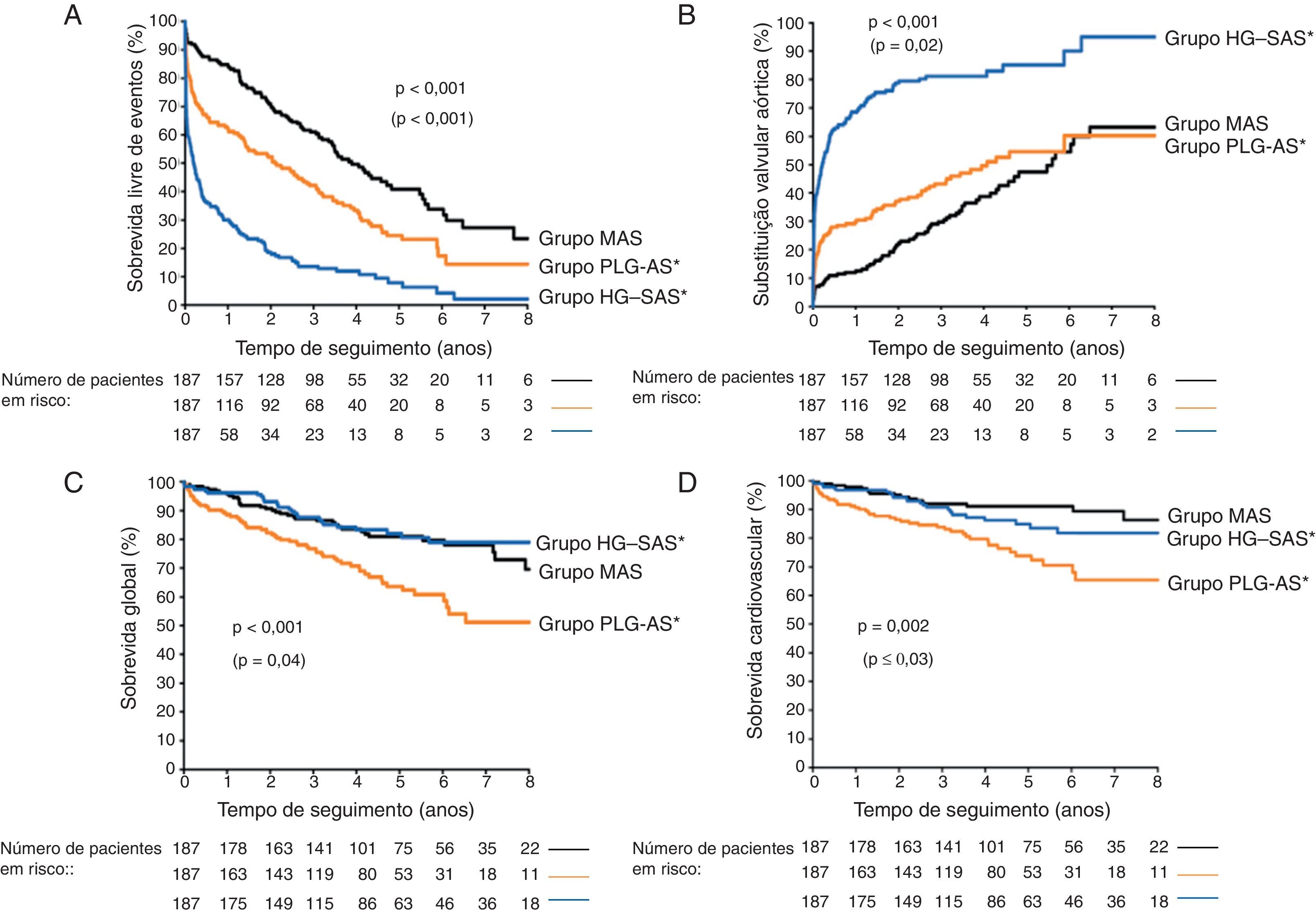
| Clavel, 201210 | Estudo retrospetivo de 1589 doentes com EA moderada a grave e FEVE>50%, divididos em três grupos, equiparados: – 187 doentes com EA paradoxal grave (AVA<1cm2/m2; GM<40mmHg, VESI≤35mL/m2, FEVE≥50%) (grupo 1); – 187 doentes com EA grave (AVA≤0,6cm2/m2; GM>40mmHg) (grupo 2); – 187 doentes com EA moderada (AVA>0,6cm2/m2) (grupo 3) | 1. Os doentes com EA paradoxal eram mais velhos, mais frequentemente mulheres e tinham maior prevalência de doença coronária e HTA, maior ZVA, FC mais rápida, SC menor, FEVE menor e um volume telediastólico do VE menor 2. Os doentes com EA paradoxal tiveram uma sobrevida (todas as causas e cardiovascular) menor a um e a cinco anos do que os doentes com EA moderada ou EA grave 3. A substituição valvular aórtica foi um preditor de sobrevida em doentes com EA paradoxal e EA grave, mas não em doentes com EA moderada 4. Os fatores independentemente associados a um aumento de morte (todas as causas) foram: idade avançada (p<0,01), tratamento conservador (p<0,01), FEVE diminuído (p=0,03) e pertencer ao grupo EA paradoxal (p=0,02) 5. O prognóstico dos doentes com EA paradoxal foi pior do que aquele dos doentes com EA grave de alto gradiente ou moderada |
| Mohty, 201317 | Estudo observacional de 768 doentes com EA grave (AVA≤1cm2) e FEVE>50%. Divididos em quatro grupos consoante GM (<versus≥40mmHg) e VESI (<versus≥35mL/m2): – fluxo normal, alto gradiente (grupo NFHG); – baixo fluxo, baixo gradiente (grupo LFLG); – baixo fluxo, alto gradiente (grupo LFHG); – fluxo normal, baixo gradiente (grupo NFLG) | 1. Dos doentes avaliados, 58% eram homens, 89% sintomáticos, 50% hipertensos e 90,7% foram submetidos a SVAC 2. A prevalência dos doentes do grupo NFHG foi de 50%, do grupo LFLG de 13%, do grupo LFHG de 15% e do grupo NFLG de 22% 3. Os doentes do grupo LFLG eram significativamente mais velhos (p<0,01), com maiores taxas de FA (p<0,01), FC mais rápida (p<0,01), FEVE mais baixa (p=0,01) e uma tendência para taxas mais elevadas de doença coronária (p=0,07), comparativamente aos outros grupos 4. O grupo LFLG apresentou RVP e ZVA significativamente mais elevadas (ambas p<0,01) do que nos outros grupos, mas uma CAS diminuída (p<0,01) 5. A SVAC foi menos frequentemente efetuada no grupo LFLG, comparativamente com os outros grupos, 84 versus 94% (NFHG), 87% (NFLG) e 91% (LFHG), (p<0,01) 6. A taxa de mortalidade operatória da SVAC tendeu a ser mais elevada no grupo LFLG (p=0,01) 7. Sobrevida a dez anos foi reduzida no grupo LFLG (32%) comparativamente com o grupo NFHG (66%), que teve o prognóstico mais favorável a dez anos 8. Após ajuste para outros fatores de risco, a condição de baixo fluxo e baixo gradiente foi independentemente associada com sobrevida reduzida a longo prazo (p<0,01) 9. Doentes do grupo LFLG demonstraram melhor sobrevida a longo prazo quando submetidos a SVAC do que a tratamento médico (p<0,01) A SVAC mostrou estar significativamente associada a melhor sobrevida no grupo LFLG (p<0,01) |
| O'Sullivan, 201356 | Estudo retrospetivo de 354 doentes com EA grave (AVAi≤0,6cm2/m2 ou GM>40mmHg) submetidos a SVAP Divididos em três grupos: – 208 doentes com GM>40mmHg (grupo 1); – 85 doentes com AVAi≤0,6cm2/m2, GM<40mmHg, VESI≤35mL/m2 e FEVE≥50% (grupo 2); – 61 doentes com AVAi≤0,6cm2/m2, GM≤40mmHg e FEVE≤40% (grupo 3) | 1. Os doentes do grupo 2 tiveram AVAi significativamente maiores, comparativamente com os outros grupos 2. Comparativamente ao grupo 1, os grupos 2 e 3 mostraram ter RVP mais elevadas (p<0,01) mas ZVA mais baixas (p=0,027) 3. A mortalidade (todas as causas e cardiovascular) a 30 dias não foi semelhante para os três grupos 4. Melhoria funcional pela classificação da NYHA a um ano ocorreu na maioria dos doentes de todos os grupos (p=0,09) 5. Não foram observadas alterações significativas da mortalidade a um ano entre os três grupos (p=0,67) |
| Eleid, 201353 | Estudo prospetivo comparativo de 24 doentes com EA grave (AVA≤1cm2 ou AVAi≤0,6cm2/m2) de baixo gradiente (<40mmHg) e sintomáticos. Divididos em dois grupos: – 18 doentes com FEVE(>50%) preservada (grupo 1); – seis doentes com FEVE(≤50%) diminuída (grupo 2) | 1. Os doentes do grupo 1 eram mais velhos e a maioria hipertensos 2. No grupo 1, todos os doentes tinham hipertensão pulmonar, pressões de enchimento ventricular elevadas e VESI diminuído 2. Os doentes do grupo 1 demonstraram uma correlação estreita entre pressão aórtica sistólica e a pressão no VE no final da diástole (r=0,64, p<0,01) 3. Não foi encontrada correlação significativa, no grupo 1, entre a pressão aórtica sistólica e o GM (r=‐0,18, p=0,29) 4. Todas as avaliações da pós‐carga ventricular esquerda melhoraram após nitroprussiato e.v. em ambos os grupos 5. O nitroprussiato e.v. diminuiu a pressão média aórtica, a pressão no VE no final da diástole e a pressão média da artéria pulmonar (p<0,05) 6. No grupo 1 o GM aumentou de 27 para 29mmHg (p=0,02) após nitroprussiato e.v., e a AVA de 0,86 para 1,02cm2 (p<0,01) |
| Herrmann, 201350 | Estudo clínico multicêntrico aleatorizado (PARTNER) de 971 doentes com EA grave (AVA<0,8cm2 ou AVAi<0,5cm2/m2 e GM≥40mmHg ou VPEA≥4,0m/s). Divididos em dois coortes: – coorte A: doentes de alto risco; – coorte B: doentes inoperáveis | 1. Cinquenta e cinco por cento dos doentes tinham baixo fluxo e 45% fluxo normal 2. Quarenta e cinco por cento dos doentes tinha baixo gradiente (≤40mmHg) 3. Vinte e três por cento dos doentes tinham baixo fluxo e FEVE diminuído (<50%) 4. Quinze por cento dos doentes tinham baixo fluxo, FEVE diminuído (<50%) e GM<40mmHg 5. A prevalência da EA paradoxal era de 31% 6. Os doentes com baixo fluxo tinham mais comorbilidades, incluindo doença coronária, pacemaker, sintomas de insuficiência cardíaca e pressões mais elevadas da artéria pulmonar do que os doentes com fluxo normal 7. A mortalidade de todas as causas a dois anos foi significativamente superior nos doentes com baixo fluxo, comparativamente ao fluxo normal (47 versus 34%, p<0,01) 8. Tratamento cirúrgico ou percutâneo esteve associado a um aumento marcado da sobrevida a um e dois anos. Comparado com tratamento médico que teve mortalidade a dois anos de 76%, a mortalidade com SVAC ou SVAP variou dos 38 aos 46% 9. A diferença no coorte B entre tratamento médico e SVAP foi estatisticamente significativa, com melhor sobrevida a dois anos para SVAP (p<0,01) 10. Não foi registada diferença significativa na sobrevida a dois anos no coorte A entre SVAC e SVAP (p=0,47) 11. Os doentes do coorte A com baixo fluxo tiveram mortalidade superior a dois anos comparativamente aos doentes com fluxo normal, quer tivessem sido submetidos a SVAC (38 versus 29%) ou SVAP (40 versus 25%) 12. Nos doentes do coorte B, aqueles com baixo fluxo apresentaram mortalidade superior do que os com fluxo normal, mas ambos melhoraram com SVAP (46 versus 76% no baixo fluxo e 38 versus 53% no fluxo normal, p<0,01) 13. Nos doentes com EA paradoxal, houve uma redução da mortalidade com SVAP comparativamente ao tratamento médico (p<0,01) 14. Nos doentes com EA paradoxal a SVAP reduziu a mortalidade a um ano de 66 para 35% (p=0,02) 15. Nos doentes com EA paradoxal não houve diferença significativa no coorte A entre SVAP e SVAC (39 versus 38,3%, p=0,69) Apenas o baixo fluxo foi um preditor independente de mortalidade em todos os coortes, enquanto a FEVE e o GM não foram significativos |
| Ozkan, 201354 | Estudo prospetivo de 260 doentes com EA grave (AVAi≤0,6cm2/m2) sintomática com GM<40mmHg e FEVE≥50% | 1. Cinquenta e três por cento dos doentes receberam tratamento médico e 47% foram submetidos a SVAC ou SVAP 2. Comparativamente aos doentes submetidos a SVAC e SVAP os doentes tratados medicamente tinham maior prevalência de diabetes, TA mais baixa, maior uso de diuréticos e níveis de creatinina superiores 3. Os doentes submetidos a SVAP eram mais velhos e tinham maior prevalência de mulheres, comparados com os doentes submetidos a SVAC 4. Comparado com os doentes de fluxo normal e baixo gradiente, os doentes com baixo fluxo e baixo gradiente tinham FEVE mais baixas (62 versus 59%, p<0,01), EA mais grave (0,46 versus 0,35cm2/m2, p<0,01) e ZVA mais elevada (3,9 versus 5,6mmHg/mL/m2, p<0,01) 5. Durante os 28±24 meses de follow‐up, 105 doentes morreram (40%): 30% nos doentes submetido a SVAC e 70% nos doentes tratados medicamente 6. SVAC mostrou estar associada a um prognóstico mais favorável (p<0,01) 7. Foi demonstrado que a SVAC está independentemente associada ao prognóstico (p<0,013) 8. Os doentes tratados medicamente tiveram uma mortalidade (todas as causas) duas vezes superior 9. Comparativamente aos doentes com fluxo normal e baixo gradiente, aqueles com baixo fluxo e baixo gradiente apresentaram sobrevida semelhante após a SVAC 10. Num modelo não ajustado de análise Kaplan‐Meier, os doentes com baixo fluxo e baixo gradiente mostraram ter pior prognóstico (p=0,007) 11. Após ajustamento para idade, género e tratamento, não houve associação entre o padrão de fluxo e o resultado clínico (p=0,64) |
| Eleid, 20137 | Estudo observacional de 1704 doentes consecutivos com EA grave (AVA<1,0cm2) e FEVE preservada (≥50%) avaliados através de ecocardiografia bidimensional Divididos em quatro grupos consoante VESI (<35mL/m2versus≥35mL/m2) e GM (<40mmHg versus≥40mmHg): – 50 doentes com baixo fluxo e alto gradiente (LF/HG); – 53 doentes com baixo fluxo e baixo gradiente (LF/LG); – 352 doentes com fluxo normal e baixo gradiente (NF/LG); – 1249 doentes com fluxo normal e alto gradiente (NF/HG) | 1. O grupo NF/LG (21%) foi associado a sobrevida mais favorável com tratamento médico (82 versus 67% no grupo NF/HG, p<0,01) 2. O grupo LF/LG (3%) foi caracterizado por VE menor, ZVA mais elevada, uma FEVE mais baixa, maior prevalência de FA e insuficiência cardíaca, CAS reduzida e sobrevida reduzida (60 versus 82% no grupo NF/HG, p<0,01) 3. Os doentes com FA eram mais velhos, com FC em repouso mais elevadas e uma prevalência aumentada de sintomas 4. A sobrevida a dois anos foi de 60% no grupo LF/LG comparado com 85% no grupo NF/LG, 82% no grupo NF/HG e 78% no grupo LF/HG (p<0,01) 5. Os doentes do grupo LF/LG tiveram a maior mortalidade de todas as causas, comparado com todos os grupos 6. O padrão de baixo fluxo e baixo gradiente foi o mais forte preditor de mortalidade (p<0,01) 7. SVAC foi associada com uma redução de mortalidade de 69% no grupo LF/LG e NF/HG (p<0,01), mas não demonstrou benefício na sobrevida dos grupos NF/LG e LF/HG |
| Mohty, 201455 | Estudo retrospetivo de 677 doentes com EA grave (AVA≤1cm2) com FEVE preservada (≥50%) e submetidos a SVAC | 1. EA paradoxal teve uma prevalência de 26% 2. Após SVAC, 54% dos doentes tiveram mismatch prótese‐doente (MPP) (AVAi≤0,85cm2/m2) 3. Dentro dos doentes com EA‐pLFLG, 56% tiveram MPP 4. Os doentes com EA‐pLFLG e MPP eram significativamente mais velhos e com mais comorbilidades, comparados com os doentes sem EA‐pLFLG e sem MPP 5. A sobrevida a dez anos foi significativamente reduzida nos doentes com EA‐pLFLG e MPP comparativamente com os doentes sem EA‐pLFLG e sem MPP (38 versus 70%, p=0,002) 6. A coexistência de EA‐pLFLG antes da cirurgia e MPP depois da cirurgia está associada a um pior prognóstico |
| Clavel, 201441 | Estudo de coorte de 400 doentes com EA moderada a grave divididos em dois coortes: – coorte A: 250 doentes consecutivos com EA paradoxal e EA grave com fluxo normal e alto gradiente (NF/HG), submetidos a SVAC; – coorte B: 150 doentes não‐consecutivos com EA moderada a grave, FEVE preservado e fluxo normal, submetidos a SVAC | 1. Os doentes com EA paradoxal tinham maior prevalência de dislipidémia e doença coronária, VESI mais baixo, cavidade ventricular esquerda mais pequena, GM mais reduzidos e ZVA mais elevada, comparativamente aos doentes com NF/HG do coorte A 2. O peso das válvulas excisadas foi menor nos doentes com EA paradoxal, bem como a prevalência do fenótipo bicúspide (15 versus 42% nos doentes NF/HG) Aplicando os valores de cut‐off de peso das válvulas excisadas como sendo grave (≥2,0g para sexo masculino e≥1,2g para sexo feminino), 70% dos doentes com EA paradoxal e 86% dos doentes com NF/HG tinham EA grave |
| Maes, 201422 | Estudo prospetivo de 349 doentes com EA grave e FEVE preservada. Doentes divididos em dois grupos de acordo com o GM: – alto gradiente (n=144), GM>40mmHg; – EA‐pLFLG (n=205), GM≤40mmHg | 1. Os doentes de ambos os grupos apresentavam características clínicas e demográficas semelhantes 2. A FA e a DM foram mais prevalentes no grupo da EA paradoxal 3. Os doentes com EA paradoxal apresentavam AVAi e IPE maiores, DVEFD e VVEFD reduzidos, VESI mais baixos e ZVA maior, comparativamente aos doentes com alto gradiente 4. A sobrevida de todas as causas a quatro anos foi superior nos doentes com EA‐EA paradoxal, em comparação com os doentes com alto gradiente 5. O GM não mostrou ter qualquer impacto significativo na sobrevida a quatro anos nos doentes com EA grave 6. Os doentes com EA paradoxal foram menos referenciados para SVAC do que aqueles com alto gradiente (7 versus 17%, p<0,01) 7. Sobrevida sem SVAC foi superior nos doentes com EA paradoxal comparativamente com os doentes de alto gradiente, na população geral em estudo (p<0,01) e na população sintomática (NYHA I ou II) (p=0,002) 8. As variáveis independentemente associadas com o resultado clínico foram: idade, volume do VE, presença de DPOC, DM e a classe NYHA 9. Nos doentes sintomáticos (NYHA classe I ou II), os fatores que foram considerados preditores independentes do resultado clínico foram: GM, idade, DM e volume do VE 10. A SVAC resultou numa melhoria significativa da sobrevida em ambos os grupos 11. A magnitude da proteção da SVAC tendeu a ser mais importante nos doentes com alto gradiente do que nos doentes com EA paradoxal, uma vez que estes apresentaram melhor resultado clínico quando não operados 12. Oitenta e dois por cento dos doentes com EA paradoxal evoluíram, ao longo do tempo, para uma forma de EA grave com aumento do GM, sendo que metade destes passaram para uma classe de EA grave de alto gradiente 13. Nos doentes do grupo de alto gradiente, a minoria que evoluiu para um estado de baixo GM, fê‐lo para uma forma «clássica» de EA baixo fluxo e baixo gradiente 14. A sobrevida em doentes com EA paradoxal melhora com a SVAC comparativamente com o tratamento médico |
| Lauten, 201457 | Estudo prospetivo de 3077 doentes consecutivos do registo Germany Aortic Valve Registry (GARY) submetidos a SVAP. Divididos em três grupos: – grupo 1: EA grave de baixo gradiente e baixo fluxo (FEVE≤40%, GM<40mmHg, AVAi≤0,6cm2/m2); – grupo 2: EA‐pLFLG (FEVE≥50%, GM<40mmHg e AVAi≤0,6cm2/m2); – grupo 3: EA grave de alto gradiente (GM≥40mmHg e AVAi≤0,6cm2/m2) | 1. O grupo 1 representava 11,7% da população em estudo, o grupo 2 (EA paradoxal) 20,8% e o grupo 3 60,6% 2. Os doentes com EA paradoxal eram ligeiramente mais novos do que os doentes do grupo 3 (p<0,01) mas mais velhos do que os doentes do grupo 1 (p=0,001), a prevalência do género feminino foi superior neste grupo e no grupo 3 3. As comorbilidades entre o grupo 2 e 3 eram semelhantes, já o grupo 1 apresentava mais comorbilidades do que os outros dois grupos de doentes 4. A mortalidade durante o internamento para realização de SVAP foi superior nos doentes do grupo 1 comparativamente ao grupo 3 (p=0,029), não havendo diferença significativa entre os doentes do grupo 2 e 3 (p=0,67) 5. Após um ano, a diferença entre a mortalidade do grupo 1 e os outros dois grupos tornou‐se mais pronunciada (32,3 versus 22,3% [grupo 2], p=0,01 e 19,8% [grupo 3], p<0,001) 6. Não houve diferença significativa entre o grupo 2 e 3 quanto à mortalidade após um ano de SVAP (p=0,192) 7. A taxa de eventos cardíacos e cerebrais major ao fim de um ano de SVAP foi superior nos doentes do grupo 1, comparativamente aos outros dois grupos (grupo 1: 34,5% versus grupo 2: 27,5% [p=0,021] e grupo 3: 23,8% [p<0,001]) 8. A mortalidade durante o internamento teve como preditores independentes a DAC de três vasos, a hipertensão pulmonar e a doença vascular periférica 9. Em particular nos doentes com EA paradoxal, a mortalidade durante o internamento teve como preditores independentes a DAC de três vasos (p=0,018) e a DPOC (p=0,005) |
AVA: área valvular aórtica; AVAi: área valvular indexada; CAS: compliance arterial sistémica; DLG: deformação longitudinal global; DM: diabetes mellitus; DPOC: doença pulmonar obstrutiva crónica; DVEFD: diâmetro do ventrículo esquerdo no final da diástole; EA: estenose aórtica; EA‐pLFLG: estenose aórtica paradoxal; FA: fibrilhação auricular; FC: frequência cardíaca; FEVE: fração de ejeção do ventrículo esquerdo; GM: gradiente médio transvalvular; IPE: índice de perda de energia; LFHG: baixo fluxo, alto gradiente; LFLG: baixo fluxo, baixo gradiente; NFHG: fluxo normal, alto gradiente; NFLG: fluxo normal, baixo gradiente; NYHA: New York heart association; RVP: resistência vascular periférica; SC: superfície corporal; SVAC: substituição valvular aórtica cirúrgica; SVAP: substituição valvular aórtica percutânea; TA: tensão arterial; TSVE: trato de saída do VE; VE: ventrículo esquerdo; VPEA: velocidade de pico de ejeção aórtica; VESI: volume ejeção sistólico indexado; VVEFD: volume do ventrículo esquerdo no final da diástole; ZVA: impedância valvulo‐arterial.
Da pesquisa realizada foram identificados 14 artigos originais sobre a EA paradoxal. Quanto ao desenho dos estudos, quatro eram retrospetivos6,8,54,55 e sete prospetivos11,16,17,22,41,52,53. Foram ainda incluídas duas subanálises de estudos aleatorizados49,51 e uma outra de um registo multicêntrico56.
Cerca de um terço dos estudos teve como objetivo a comparação dos doentes com EA paradoxal com o fenótipo clássico da EA6,8,11,22,51. Um estudo incluiu a comparação com o grupo de doentes com EA moderada8 e outro uma comparação com o grupo da EA‐BFBG52. Dois estudos avaliaram a interação entre o gradiente valvular e o VESI para doentes com AVA≤1cm2 e FEVE≥50% (16,17). Para além disso, seis estudos centraram‐se na terapêutica cirúrgica6,8,16,17,22,53 e outros três no tratamento percutâneo dos doentes com EA paradoxal49,55,56. Estes 14 artigos são resumidos na Tabela 1.
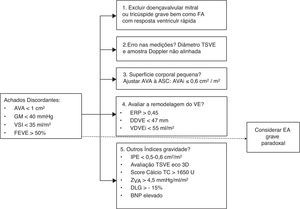
DefiniçãoA EA paradoxal é definida concretamente por uma AVA ≤1cm2, com GM<40mmHg e um VESI ≤35mL/m2, isto apesar de uma FEVE≥50% (Figura 1)8. Este contexto é geralmente o resultado de uma remodelagem concêntrica marcada do VE, com fibrose miocárdica intersticial, redução da cavidade ventricular e da compliance da câmara8,11–15. No entanto, apesar de uma boa função sistólica global do VE no fenótipo da EA paradoxal, foi reconhecida uma diminuição da mecânica miocárdica longitudinal do VE6.
O estado de baixo fluxo sistólico dificulta a correta avaliação da gravidade da estenose valvular aórtica, uma vez que o gradiente é uma função quadrática do fluxo. Assim, qualquer diminuição do fluxo implica uma acentuada diminuição do gradiente e por conseguinte uma subestimação da gravidade da doença9. Para além disso, a taxa de fluxo transvalvular não depende apenas do volume de ejeção mas também do tempo de ejeção19. No entanto, outros fatores como a fibrilhação auricular (FA), a regurgitação mitral, a estenose mitral e a regurgitação tricúspide podem desempenhar um importante papel na redução do volume de ejeção sistólico, contribuindo também para um estado de baixo fluxo e de gradientes valvulares reduzidos7,16.
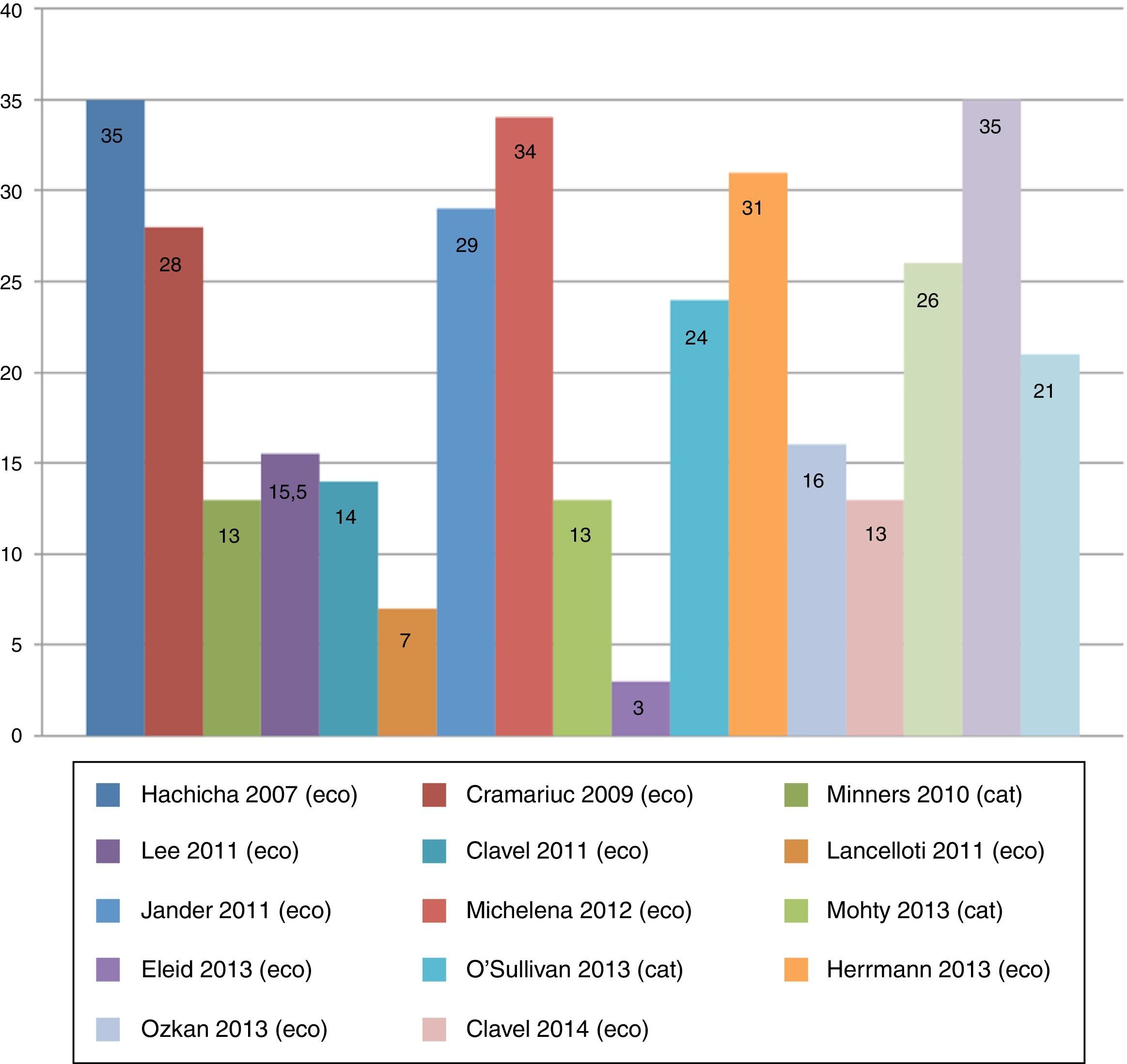
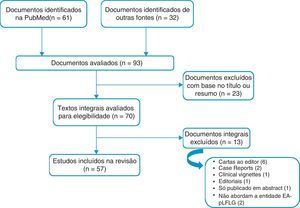
Características clínicasExiste uma variabilidade na prevalência da EA paradoxal de 3‐35% da população com EA degenerativa grave (Figura 2)6,7. Tal discrepância pode ser devida às características das amostras selecionadas8,16. Assim, Eleid et al.7, num estudo ecocardiográfico de 1704 doentes consecutivos com EA grave e FEVE preservada (≥50%), encontraram uma prevalência de apenas 3% de doentes com EA paradoxal. Pelo contrário, Kusunose et al.6, num outro estudo ecocardiográfico de 397 doentes com EA, documentaram uma prevalência de 35% de doentes com EA paradoxal. Uma outra análise, com uma amostra baseada em doentes referenciados para cateterismo cardíaco, revelou prevalência da EA paradoxal de 26% dos casos de EA grave17, concordante com os estudos ecocardiográficos.
A EA paradoxal parece ser mais frequente no género feminino e nos doentes com idade mais avançada. Em comparação com a forma clássica de EA grave com GM elevado, está associada a uma maior proporção de doentes com antecedentes de hipertensão arterial (HTA), diabetes, FA e doença coronária6,7,9,10,17,18. A HTA é frequente nos doentes com EA, no entanto, a tensão arterial (TA) nos doentes com EA paradoxal pode estar pseudonormalizada pelo padrão de baixo fluxo sistólico associado a uma rigidez vascular aumentada8. A sintomatologia é consistente com aquela da EA grave clássica, embora seja considerada uma doença de instalação mais insidiosa1,10.
Métodos diagnósticos da estenose aórtica paradoxalNa suspeita de EA paradoxal, para além da VPEA, dos gradientes transvalvulares aórticos e da AVA é sugerida uma avaliação que considere: a carga vascular; a carga hemodinâmica global do VE; o desempenho do VE para além da FEVE; a geometria do VE e o dano miocárdico19.
A ecocardiografia transtorácica é o método de escolha para o estudo hemodinâmico na EA. Não está indicada a utilização por rotina do cateterismo cardíaco, a não ser nos casos em que a ecocardiografia seja não diagnóstica ou em que haja discrepância com os dados clínicos20,21.
Problemática relacionada com o cálculo da área valvular aórticaA AVA é calculada pela equação de continuidade que deriva dos princípios de conservação de massa. Assim, assume‐se que o volume que passa numa determinada área a montante da válvula aórtica é o mesmo que passa através da válvula. Esta medição é menos dependente do fluxo do que outros parâmetros como a velocidade e os gradientes, mas é suscetível à ocorrência de erros, dado que é uma medida indireta da área valvular. Em primeiro lugar, a equação de continuidade avalia o tamanho do orifício funcional e não do anatómico, uma vez que não leva em consideração o coeficiente de contração orificial. Assim, e em condições de fluxo normal, pensa‐se que a subestimação do orifício anatómico por esta equação seja na ordem dos 10‐15%22. Por outro lado, o volume de ejeção sistólico do VE (numerador da equação de continuidade) é geralmente calculado da ecocardiografia bidimensional, a partir de uma área de secção, assumindo portanto uma forma circular do trato de saída do ventrículo esquerdo (TSVE). Na verdade, Doddamani et al. verificaram, com o recurso à tomografia computadorizada (TC) por multidetetores23 e ecocardiografia tridimensional24, que o TSVE é mais frequentemente elipsoide do que circular. Esta imprecisão pode resultar numa subestimação da AVA próxima dos 15%24.
Uma vez que a gravidade da EA pode ser sub ou sobrestimada caso o doente tenha, respetivamente, uma grande ou pequena área de superfície corporal (SC), torna‐se essencial indexar a área valvular à área de SC (AVAi), embora se assinale que nos extremos da SC a indexação pode não ser apropriada1.
A avaliação da consistência entre os critérios ecocardiográficos para estratificar a gravidade da EA (AVA por equação da continuidade, VPEA e GM), foi estabelecida após uma análise de 3482 ecocardiogramas de doentes com uma boa função sistólica global do VE e uma AVA<2 cm2. Foi demonstrado que o critério da AVA ≤1cm2 sobrestimou a gravidade da EA, em comparação aos outros dois (VPEA ≥4m/s; GM ≥40mmHg). Assim, os autores sugeriram que o ponto de corte da AVA para definir a EA grave deveria ser<0,8cm2, que corresponderia mais frequentemente a uma VPEA ≥4m/s e a um GM ≥40mmHg. Assinala‐se como limitação que os autores não apresentaram resultados clínicos desta reclassificação25.
Em resumo, apesar de a AVA ser um parâmetro essencial para a estratificação da gravidade de um doente com EA, é uma metodologia com limitações importantes.
A ecocardiografia tridimensional surge como uma alternativa à avaliação da AVA pela equação de continuidade26. Foi demonstrada uma maior acurácia na avaliação da AVA e na classificação da gravidade da EA por ecocardiografia tridimensional, comparativamente à equação de continuidade e aos métodos volumétricos por ecocardiografia bidimensional26.
A AVA projetada (AVAproj) é uma outra forma de estimar a AVA, aplicada na situação em que há um baixo fluxo sistólico e geralmente disfunção sistólica associada. É baseada no cálculo da AVA a um fluxo sistólico considerado normal (250ml/ms) através da fórmula AVAproj=AVAresouso+CV (250x Qrepouso), em que CV representa a compliance valvular e Qrepouso o fluxo sistólico de ejeção em repouso. A AVAproj parece representar uma boa alternativa aos parâmetros ecocardiográficos obtidos durante uma ecocardiografia de sobrecarga farmacológica com dobutamina27.
Importância da avaliação do componente vascularNos doentes com EA paradoxal as alterações vasculares são particularmente significativas. É recomendada a avaliação concomitante da TA periférica e é também sugerida a estimativa da compliance arterial sistémica (CAS) e das resistências vasculares periféricas (RVP)19. É importante assinalar que a avaliação ecocardiográfica de um doente com fluxo sistólico reduzido deverá ser realizada sob um perfil tensional controlado19,28.
A impedância valvuloarterial (ZVA) avalia de forma simples e não invasiva o conceito da dupla carga hemodinâmica (vascular e valvular) sobre o VE. É calculada dividindo a pressão sistólica do VE (pressão arterial sistólica+gradiente médio transvalvular) pelo VESI29,30. Foi demonstrado que este parâmetro tem valor prognóstico29, bem como é um bom marcador de disfunção miocárdica31. Foi recentemente publicada uma subanálise do estudo multicêntrico Simvastatin Ezetimib in Aortic Stenosis (SEAS)32, em que a ZVA foi considerada a principal determinante de disfunção ventricular em doentes assintomáticos com EA grave. Hachicha et al.29, num estudo retrospetivo, identificaram um valor de ZVA>4,5mmHg/ml m2 como indicativo de uma pós‐carga do VE gravemente aumentada, estando associado a um aumento de 2,8 e 3,7 vezes da mortalidade de todas as causas e causa cardiovascular, respetivamente. Neste mesmo estudo, a elevação da ZVA foi notória em 72% dos doentes com EA paradoxal29, tendo sido posteriormente documentado que os doentes com EA paradoxal apresentaram uma ZVA superior, em comparação com os doentes com EA grave clássica10. Em contraponto, foi estimado que a ZVA não foi um bom preditor de mortalidade a longo prazo após o tratamento cirúrgico30.
Quantificação da função intrínseca do ventrículo esquerdoA disfunção ventricular sistólica avaliada pela FEVE é uma recomendação classe I para a substituição valvular aórtica em doentes com EA grave, independentemente da sintomatologia associada, de acordo com as recomendações europeias e americanas1,3. Apesar de muito utilizada, é suscetível a erros de medição e está longe de ser considerada um indicador preciso da contratilidade do VE19. Esta observação traduz a necessidade de uma avaliação mais discriminativa da função ventricular, em particular nos doentes com EA paradoxal recorrendo a outros parâmetros19.
A deformação longitudinal global (DLG) é uma forma de complementar a avaliação da função miocárdica, baseada na metodologia de speckle‐tracking33. Este parâmetro parece menos influenciado pela geometria do VE, e é considerado superior à FEVE na avaliação e quantificação da função miocárdica intrínseca19. Vários estudos têm vindo a demonstrar que o DLG é um marcador precoce de disfunção do VE, que diminui gradualmente com a progressão da gravidade de EA19. No estudo de Lancellotti et al.34, um valor de DLG ≤15,9% associou‐se a uma taxa mais elevada de eventos cardiovasculares em doentes com EA. A heterogeneidade segmentar da DLG foi demonstrada no contexto da EA35, sendo a redução da DLG mais evidente nos segmentos basais. O uso dos parâmetros de deformação global e regional na EA paradoxal não está totalmente esclarecido, existindo uma falta de consenso sobre o valor adicional destes parâmetros no diagnóstico, estratificação de risco e prognóstico. No entanto, no estudo de Kusunose et al.6, a DLG foi um fator preditor independente de mortalidade (HR 1,05; intervalo de confiança 95% 1,03‐1.07; p<0,01), sendo que um ponto de corte de ‐12,1% esteve associado a um aumento significativo da ocorrência de morte. As mesmas conclusões formam observadas por Sato et al.36, embora com um valor discriminativo de ‐17% para a previsão de eventos cardiovasculares. Assim, estes autores sugerem que a avaliação da DLG em doentes com EA paradoxal possa vir a ter um papel importante na estratificação de risco.
Avaliação do dano miocárdicoO stress prolongado sobre as fibras miocárdicas leva a dano celular e morte por apoptose. A fibrose miocárdica intersticial é, portanto, um achado habitual na ressonância magnética cardíaca e no estudo histológico19, e está associada a um risco de manutenção da disfunção do VE mesmo após substituição cirúrgica da válvula aórtica37.
Os biomarcadores de fácil acesso como o brain natriuretic peptide (BNP) e o N‐terminal pro‐brain natriuretic peptide (NT‐proBNP) refletem a disfunção sistólica e diastólica do VE de tal modo que, quanto maior a sua elevação, mais grave a sintomatologia e pior o prognóstico37,38. Convém assinalar que os peptídeos não avaliam a gravidade da EA diretamente, mas sim o desempenho miocárdico, não sendo portanto específicos da EA19,38.
Novos parâmetros de avaliação da estenose aórtica paradoxalAtualmente, novos índices de avaliação da EA têm surgido para melhorar a compreensão desta doença.
O grau de calcificação da válvula aórtica é um forte preditor da rápida progressão da doença19. Apesar de poder ser avaliado semiquantitativamente através da ecocardiografia, a TC permite uma análise mais precisa e quantitativa do grau de calcificação19. Um score de cálcio>1000AU confirma uma calcificação grave da válvula aórtica, de acordo com as recomendações americanas de cardiologia3. Este método não é influenciado pelas características hemodinâmicas, tendo por isso utilidade na avaliação de estados de baixo fluxo, como na EA paradoxal39. Messika‐Zeitoun et al.40 demonstraram uma forte associação entre a calcificação aórtica e a AVA (r=‐0,79, p<0,01)40.
Clavel et al., num estudo de 250 doentes consecutivos submetidos a substituição valvular aórtica cirúrgica (SVAC), avaliaram o peso das válvulas excisadas41. Em 70% dos doentes com EA paradoxal a EA aórtica foi considerada grave, com base no peso das válvulas aórticas retiradas durante a cirurgia de substituição valvular. Tratou‐se de uma percentagem semelhante à encontrada nos doentes com a EA grave clássica de alto gradiente (86%)41. Este estudo reafirma que uma grande proporção de doentes com EA paradoxal têm, efetivamente, uma forma grave de EA, e aponta limitações aos métodos ecocardiográficos, nomeadamente aos gradientes valvulares para a estratificação dos doentes com EA41.
As recomendações atuais não diferenciam entre a forma de quantificação da AVA, ou por cateterismo ou por ecocardiografia com Doppler. A determinação da AVA pode ser realizada de forma invasiva, através da fórmula de Gorlin20. Assinala‐se que esta fórmula é dependente do fluxo sistólico e é considerada pouco adequada para a avaliação de estados de débito cardíaco reduzido. O método baseado no Doppler estima o gradiente de pressão através da válvula, a partir do valor máximo da velocidade do fluxo sistólico, ao nível da vena contracta, enquanto o método invasivo determina o gradiente de pressão entre o VE e a Ao ascendente, a vários centímetros da válvula19. A energia total do fluxo sistólico aórtico advém da energia cinética e estática (pressão). A convergência de fluxo através da válvula estenótica converte a energia estática em energia cinética, com uma redução da pressão ao nível da vena contracta. Quando a velocidade diminui distalmente à estenose, parte da energia é convertida de novo em energia estática devido a um fenómeno chamado recuperação de pressão42. A implicação clínica do fenómeno da recuperação de pressão é que a AVA calculada por Doppler é subestimada em relação à AVA calculada por método invasivo28. Para ultrapassar esta limitação, Garcia et al., em 2003, desenvolveram um novo índice, denominado índice de perda de energia (IPE)43, para ajustar a medição da AVA ao fenómeno da recuperação da pressão na Ao torácica ascendente28. O IPE calculado pela fórmula: (AVAxAA/AA–AVA), em que AA é a área da Ao torácica ascendente, medida 1cm após a junção sinotubular19,43. Este índice mostrou ter uma boa associação ao prognóstico dos doentes com EA grave, particularmente quando ≤0,6cm2/m244. Na EA paradoxal, este índice revela utilidade, aproximando‐se de medições da AVA pelo estudo invasivo, e parecendo acrescentar um significado prognóstico28, sendo que alguns autores sugerem o seu uso de forma rotineira na avaliação da gravidade da EA, particularmente na presença de uma diâmetro reduzido da Ao torácica (<30mm)42.
Tal como referido previamente, EA é atualmente considerada uma doença vascular sistémica, com aumento da rigidez vascular sistémica. Estudos recentes demonstraram que é possível avaliar a mecânica vascular da Ao por ecocardiografia com a metodologia de speckle tracking – marcador imagiológico da rigidez vascular45,46. Foi demonstrado que os doentes com EA apresentam valores de mecânica da Ao reduzidos, quando comparado aos doentes com insuficiência aórtica45. Para além disso, os doentes com EA moderada a grave e baixo fluxo de ejeção apresentaram valores mais reduzidos da mecânica da Ao, do que aqueles com fluxo sistólico considerado normal46. A avaliação da mecânica vascular por speckle‐tracking apesar de promissora é uma metodologia apenas investigacional, dadas as limitações relacionadas com a necessidade de uma boa janela acústica da Ao e do tempo prolongado para análise.
Novos marcadores, como neuro‐hormonas, adipocinas e moduladores da matriz extracelular, têm sido recentemente identificados como fatores prognósticos e diagnósticos da EA grave com FEVE preservada, baixo fluxo e alto gradiente47. A sua utilidade no futuro para a abordagem dos doentes com EA‐paradoxal poderá ser também alvo de investigação.
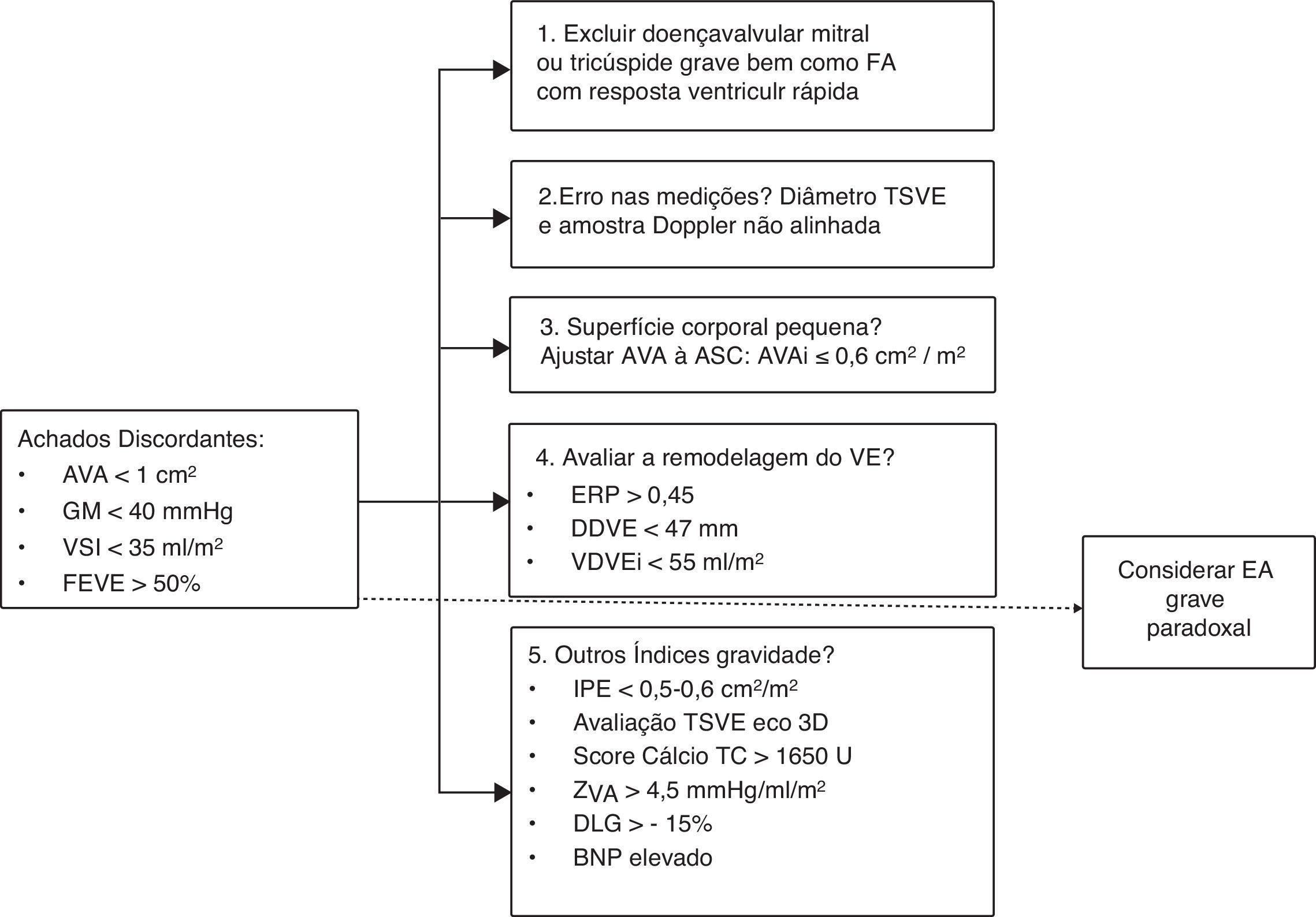
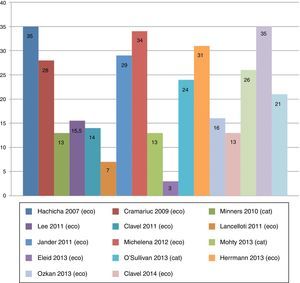
Abordagem diagnósticaQuando na avaliação de um doente com EA existirem valores discordantes entre a AVA e o GM (AVA ≤1cm2 e GM<40mmHg), num contexto de boa função sistólica do VE mas com reduzido fluxo sistólico de ejeção (VESI ≤35ml/m2), deve ser equacionada a hipótese de EA paradoxal. De acordo com Pibarot et al., em 201248, torna‐se essencial uma abordagem sistematizada (Figura 3). Desde logo, será necessário excluir multimorbilidade associada (doença valvular mitral e tricúspide significativas), erros de medição e o incorreto alinhamento da amostra Doppler. A avaliação ecocardiográfica deve ser realizada sob perfil normotensivo. A AVA deve ser indexada à SC e valorizada tendo em conta o IMC, sendo que um valor ≤0,6cm2/m2 traduz uma EA grave. São achados sugestivos de EA paradoxal grave sinais de remodelagem do VE. Nos casos em que a gravidade da EA não está totalmente estabelecida, informação adicional pode ser obtida através da avaliação de outros parâmetros, como o score de cálcio da válvula aórtica, da AVA anatómica, da ZVA, do IPE e dos índices de deformação, que ao estarem alterados são sugestivos de gravidade e, neste contexto, de EA paradoxal19.
Esquema de abordagem diagnóstica da EA paradoxal, adaptado de Pibarot et al.48. Legenda: AVA: área valvular aórtica; AVAi: área valvular aórtica indexada à superfície corporal; ASC: área de superfície corporal; BNP: péptido natriurético cerebral; DDVE: diâmetro diastólico do ventrículo esquerdo; DLG: deformação longitudinal global; EA: estenose aórtica; ERP: espessura relativa das paredes; FEVE: fração de ejeção ventricular esquerda; GM: gradiente médio; IPE: índice de perda de energia; TC: tomografia computorizada; TSVE: trato de saída do ventrículo esquerdo; VDVEi: volume diastólico do ventrículo esquerdo indexado à área de superfície corporal; VE: ventrículo esquerdo; VSI: volume de ejeção indexado; ZVA: impedância valvuloarterial.
Vários estudos apontam que o fenótipo de baixo fluxo sistólico e o baixo gradiente transvalvular, na presença de uma boa função sistólica global, possam ser marcadores de um mau prognóstico. Assim,
- •
Hachicha et al.8, num estudo retrospetivo de 512 doentes consecutivos com EA grave e FEVE preservada, demonstraram que um estado de baixo fluxo (VESI ≤35mL/m2) esteve associado a um pior prognóstico ao final de três anos;
- •
Mohty et al.17 observaram em 768 doentes com EA grave e FEVE preservada que a condição de baixo fluxo e baixo gradiente, após ajuste para outros fatores, estava independentemente associada a uma sobrevida reduzida a longo prazo;
- •
Eleid et al.7 demonstraram, com um estudo observacional de 1704 doentes consecutivos com EA grave e FEVE preservada, que o padrão fenotípico de baixo fluxo e baixo gradiente foi o mais forte preditor de mortalidade;
- •
Lancellotti et al.49, num estudo prospetivo de 150 doentes consecutivos com EA grave, mostraram que os doentes com baixo fluxo e baixo gradiente tiveram um pior resultado clínico, comparativamente aos doentes de fluxo normal e baixo gradiente. Tanto o baixo fluxo como o baixo gradiente foram considerados preditores independentes de mau prognóstico;
- •
Herrmann et al.50, no estudo Placement of AoRTic TraNscathetER Valve Trial Edwards SAPIEN Transcatheter Heart Valve (PARTNER), de 971 doentes com EA grave, demonstraram que apenas o baixo fluxo era preditor independente de mortalidade em todos os coortes (coorte A: doentes de alto risco, coorte B: doentes inoperáveis). Para além disso, foi demonstrado que a mortalidade de todas as causas a dois anos foi significativamente superior nos doentes com baixo fluxo, comparativamente com aqueles de fluxo normal.
É, portanto, relativamente consensual na literatura que os estados de fluxo sistólico reduzido, em contexto de EA grave e boa função sistólica global, estejam associados a um pior prognóstico a médio‐longo prazo10. Os eventos cardiovasculares ocorreram mais frequentemente em doentes com EA paradoxal do que naqueles com EA e fluxo normal13,51. Foi também constatado que a sobrevida a um e a cinco anos destes doentes é menor do que nos doentes com EA moderada, de acordo com um estudo retrospetivo de 1589 doentes de Clavel et al.10.
De salientar no entanto, um perspetiva diferente. Num estudo recente, Maes et al.22 avaliaram prospetivamente 349 doentes com EA grave e FEVE preservada, dividindo os doentes em dois grupos consoante o GM (> ou ≤40mmHg). Foi demonstrado que a sobrevida de todas as causas a quatro anos foi superior nos doentes com EA paradoxal, em comparação com doentes com EA grave clássica de alto gradiente. Assim, neste estudo22, o prognóstico dos doentes com EA paradoxal foi mais favorável, particularmente quando comparado com o prognóstico dos doentes com EA grave e alto gradiente.
Concordante com este estudo, um trabalho de Jander et al.52, baseado numa subanálise do estudo SEAS, demonstrou que os doentes com EA paradoxal tiveram um resultado clínico semelhante ao dos doentes com EA moderada.
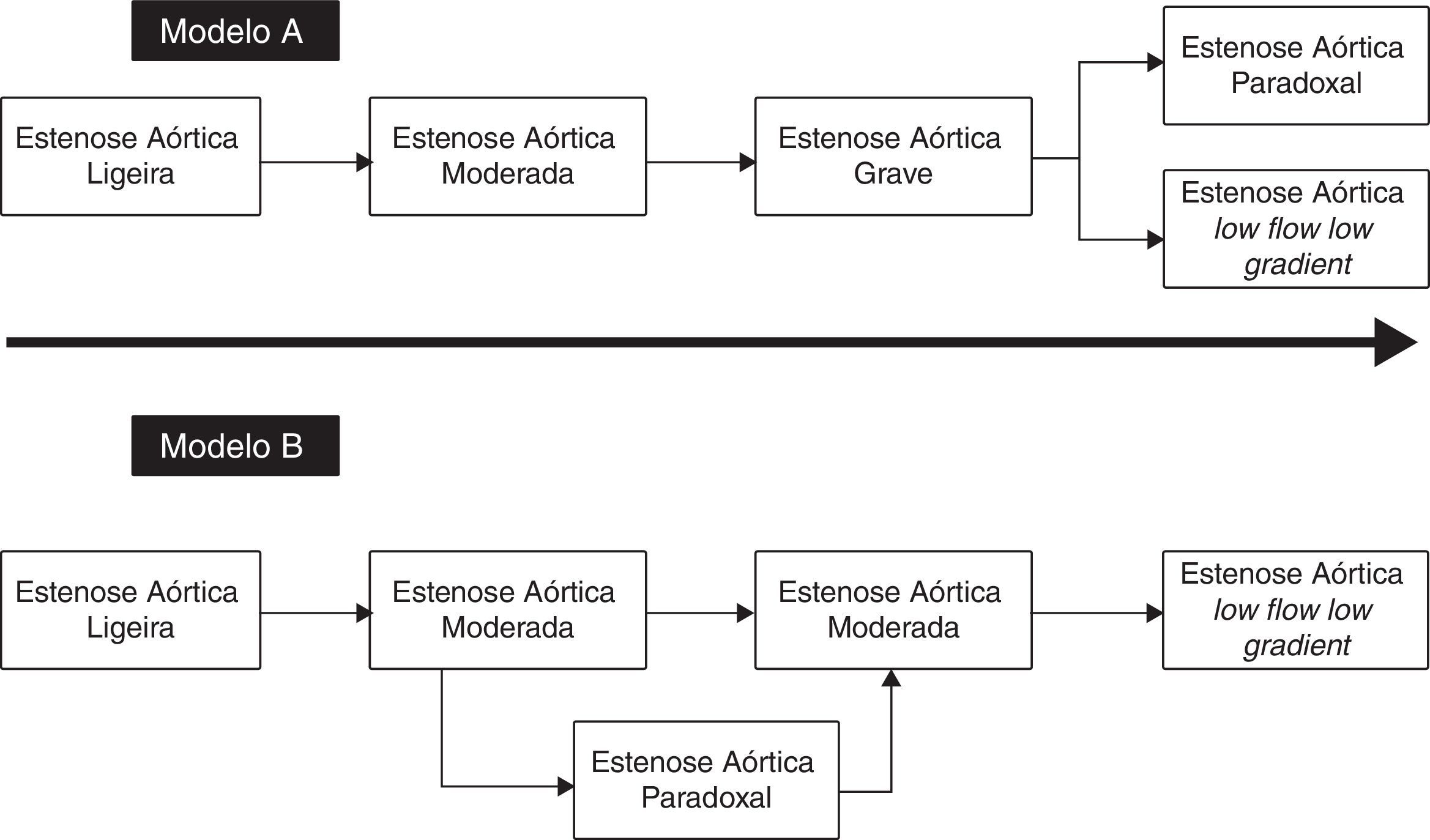
História naturalA história natural dos doentes com EA paradoxal tem sido objeto de intensa discussão desde 2007 e, como referido no final da secção anterior, parece existir uma mudança no paradigma da doença. Assim, como descrito no modelo A (Figura 4), após uma fase em que a EA atinge critérios de gravidade e na ausência de tratamento específico, o doente poderá evoluir do ponto de vista fenotípico para uma forma em que predomina a dilatação e a disfunção sistólica VE, com redução subsequente do fluxo sistólico e dos gradientes transvalvulares. Os trabalhos iniciais de Hachicha et al.8 e de Lancellotti et al.49 sugerem que os doentes com EA grave possam evoluir também para uma forma fenotípica diferente. Desta forma, a EA paradoxal representa uma fase muito avançada de doença valvular aórtica, à custa de uma marcada fibrose intersticial do VE, uma redução do tamanho da cavidade e um aumento da rigidez vascular sistémica. Tais alterações condicionam uma redução do fluxo sistólico de ejeção do VE, com uma consequente diminuição dos gradientes e da abertura valvular aórtica. Como descrito previamente, o facto dos doentes com EA paradoxal apresentarem um pior prognóstico, quando comparados com os doentes com EA clássica grave (alto gradiente) corrobora este modelo.
Dados recentes apontam, no entanto, para uma evolução diferente da doença – modelo B (Figura 4). Maes et al.22 sugerem que os doentes com EA paradoxal representam um estádio intermédio na progressão para uma forma de EA grave com gradientes elevados. O prognóstico dos doentes com EA paradoxal assemelha‐se aos doentes com EA moderada e é melhor do que nas formas graves (com alto gradiente) da EA. Para além disso, os doentes com EA grave evoluem, na ausência de um tratamento de substituição valvular, para um fenótipo de baixo fluxo, baixo gradiente, e não para uma forma paradoxal. De acordo com estes autores, provavelmente o conceito de EA paradoxal será o resultado das imprecisões da equação de continuidade para o cálculo da AVA discutidas acima.
TratamentoA EA paradoxal não pode ser analisada como uma doença isolada da válvula aórtica, mas antes uma doença vascular sistémica envolvendo um processo de atero e de arterioloesclerose. Para além disso, as manifestações clínicas na EA dependem também da remodelagem ventricular e de um bom desempenho do VE8. O tratamento deve, então, ser dirigido a todos esses fatores8.
Componente vascularQuanto ao componente vascular, de um ponto de vista clínico, será importante otimizar a TA8,53. O tratamento anti‐hipertensor diminui a pós‐carga, reduz as pressões de enchimento do VE, bem como diminui a pressão a nível das artérias pulmonares53. De acordo com as recomendações europeias e americanas1,3, não há preferência por uma ou outra classe de fármacos anti‐hipertensores nos doentes com EA. Ainda assim, nos doentes com EA paradoxal é necessário precaução com o uso de diuréticos, pela redução importante da pré‐carga, que pode gerar ainda maior redução do volume de ejeção sistólico. O uso de fármacos vasodilatadores arteriais aparentemente não tem contraindicação neste grupo de doentes. Esse conceito provém, no entanto, de um estudo em contexto agudo, com o uso de um fármaco por via endovenosa, o nitroprussiato de sódio. Assim, Eleid et al.53, num estudo prospetivo de 24 doentes, demonstraram que a utilização do nitroprussiato de sódio resultou na diminuição da pós‐carga global do VE em doentes com EA paradoxal, sem efeitos secundários significativos.
Componente valvularComo foi previamente referido, a EA grave paradoxal pode ser indicativa de um estádio de doença mais avançado e, portanto, com um pior prognóstico8,41,50. Assim, na presença de sintomatologia típica e ausência de contraindicações, os doentes devem ser submetidos a SVAC8,17,41,50,54. De acordo com as recomendações europeias e americanas, para casos sintomáticos confirmados de EA grave, com baixo fluxo e baixo gradiente apesar de FEVE preservada, a SVAC é uma recomendação de classe IIa1,3. No entanto, foi constatado que os doentes com EA paradoxal são menos vezes referenciados para cirurgia8,10,17,28. Tal acontece quer pela subestimação da gravidade da EA pelos métodos de avaliação rotineiramente utilizados (velocidade de ejeção do VE, GM e área valvular), quer pelo contexto epidemiológico da doença10,17,41.
Substituição valvular aórtica cirúrgicaNos doentes com EA paradoxal, a SVAC mostrou ser superior ao tratamento médico, bem como melhorou o prognóstico. Tal é corroborado por diversos autores, assim:
- •
Hachicha et al.8, num estudo retrospetivo de 512 doentes consecutivos com EA grave e FEVE preservada, observaram que os doentes com baixo fluxo tratados medicamente tiveram pior prognóstico a três anos do que aqueles tratados cirurgicamente (58 versus 93%, p<0,01);
- •
Clavel et al.10 demonstraram, num estudo retrospetivo de 1589 doentes com EA moderada a grave e FEVE>50%, que a SVAC foi um preditor independente de sobrevida no grupo com EA‐paradoxal (Figura 5);
Figura 5.Análise Kaplan‐Meier combinada de eventos, SVAC, sobrevida global e sobrevida cardiovascular. Figura do estudo de Clavel et al.10, publicado com a permissão da Elsevier. Nesta análise é possível observar que, em A, a sobrevida livre de eventos a um e a cinco anos de seguimento foi de 63 e 24%, respetivamente para EA paradoxal, versus 30 e 9%, para a EA grave e alto gradiente, e 85 e 41% para a EA moderada (p<0,01). Em B, é possível constatar que o grupo de doentes com EA paradoxal foi menos referenciado para SVAC, comparativamente com os doentes com EA grave e alto gradiente. No entanto, foram submetidos a SVAC mais frequentemente do que os doentes com EA moderada10. Quanto à sobrevida global e cardiovascular, observada em C e D, esta foi mais reduzida para os doentes com EA paradoxal comparativamente aos doentes com EA grave de alto gradiente e EA moderada. HG‐SAS, estenose aórtica severa alto gradiente; MAS, estenose aórtica moderada; PLG‐AS, estenose aórtica paradoxa. * Valor de p estatisticamente significativo (p < 0,05) em comparação com o grupo de doente com estenose aórtica moderada.
(0,41MB). - •
Mohty et al.17, num estudo observacional de 768 doentes com EA grave e FEVE>50%, divididos em quatro grupos consoante o GM (< versus ≥40mmHg e o VESI<versus ≥35mL/m2), descreveram que os doentes com baixo fluxo e baixo gradiente apresentaram melhor sobrevida a longo prazo quando submetidos a SVAC, em comparação com os doentes que permanecem em tratamento médico;
- •
Ozkan et al.54 demonstraram, num estudo prospetivo de 260 doentes com EA grave sintomática, GM<40mmHg e FEVE ≥50%, que a SVAC esteve associada a um prognóstico mais favorável, sendo que os doentes tratados medicamente tiveram uma mortalidade duas vezes superior aos submetidos a SVAC;
- •
Eleid et al.7, num estudo observacional de 1704 doentes consecutivos com EA grave e FEVE preservada, divididos em quatro grupos consoante o VESI e o GM, demonstraram que a SVAC foi associada a uma redução da mortalidade no grupo de doentes com baixo fluxo e baixo gradiente.
No entanto, Maes et al.22, num estudo prospetivo de 349 doentes com EA grave e FEVE preservada, demonstraram que a sobrevida sem tratamento cirúrgico (SVAC) foi superior nos doentes com EA paradoxal, comparativamente aos doentes com EA grave clássica de alto gradiente. Assinala‐se que, neste estudo, o estado de baixo fluxo sistólico do VE não influenciou o prognóstico. Apesar disso, quando submetidos a SVAC, todos os grupos de doentes demonstraram melhoria significativa da sobrevida22. No mesmo estudo22, referem ainda que a sobrevida em doentes com EA paradoxal melhora com SVAC, comparativamente com o tratamento médico.
Importa referir, contudo, que a mortalidade operatória dos doentes com EA paradoxal é superior quando comparada com os doentes com EA grave de alto gradiente17. As causas prováveis para esse aumento de mortalidade prendem‐se com a idade mais avançada, maior multimorbilidade cardiovascular e não cardiovascular, e, como explicado previamente, a um possível estádio mais avançado de doença17. Para além disso, os doentes com EA paradoxal são suscetíveis a um mismatch entre o doente e a prótese (PPM) (AVAi ≤0,85cm2/m2), sendo a combinação de EA paradoxal e mismatch pós‐operatório associada a um pior prognóstico55.
Substituição valvular aórtica percutâneaNos doentes que não apresentam condições (contraindicação ou alto risco cirúrgico) para serem submetidos a SVAC, a substituição valvular aórtica percutânea (SVAP) pode também ser uma alternativa1. A SVAP demonstrou melhores resultados em termos prognósticos e de sobrevida a longo prazo, comparativamente ao tratamento médico, obtendo resultados nos doentes com EA paradoxal comparáveis aos doentes com EA grave clássica, como mostram os seguintes estudos:
- •
O'Sullivan et al.56, num estudo retrospetivo de 354 doentes com EA grave submetidos a SVAP, demonstraram que a SVAP em doentes com EA paradoxal teve taxas de mortalidade comparáveis às da EA grave clássica;
- •
Herrmann et al.50, numa análise do estudo PARTNER de 971 doentes aleatorizados com EA grave, demonstraram que nos doentes com EA paradoxal a SVAP apresentou uma redução da mortalidade comparativamente ao tratamento médico, de 73% para 43% (p<0,01), em doentes inoperáveis;
- •
Lauten et al.57, num estudo prospetivo de 3077 doentes consecutivos do registo Germany Aortic Valve Registry (GARY), submetidos a SVAP, demonstraram que o resultado clínico entre os doentes com EA paradoxal e EA grave clássica é comparável, não havendo diferença significativa entre estes dois grupos de doentes quanto à mortalidade um ano após o procedimento.
A decisão de optar pelo SVAP nos doentes com EA paradoxal depende de um grupo de trabalho multidisciplinar (Heart Team), que define, localmente e caso a acaso, as indicações e contraindicações para a substituição valvular aórtica1. Assinala‐se ainda que de uma outra análise do estudo PARTNER não foram registadas diferenças significativas na mortalidade em doentes de alto risco entre SVAC e SVAP (39 versus 38,3%, p=0,69), mantendo em aberto a discussão sobre qual o melhor método terapêutico nos doentes com EA paradoxal49.
De uma forma resumida, a literatura parece relativamente unânime quanto à necessidade de substituição valvular aórtica (cirúrgica ou percutânea), num doente sintomático com EA paradoxal1. Tal como foi desenvolvido acima, ambas as opções demonstraram uma melhoria do prognóstico, da sobrevida e do resultado clínico em doentes com EA paradoxal comparativamente com o tratamento médico. A decisão do método terapêutico final dependerá da avaliação do risco cirúrgico do doente e das condições logísticas de cada centro1.
DiscussãoA EA paradoxal foi descrita pela primeira vez em 2007 e as características fenotípicas foram corroboradas por diferentes grupos. Há, no entanto, questões relacionadas com as inconsistências da equação da continuidade e o cálculo da AVA que podem explicar os achados discordantes característicos deste fenótipo e reclassificar formas de EA grave em EA moderada. Assim, surgiram outros métodos de diagnósticos não invasivos, importantes para corroborar o fenótipo paradoxal de EA grave, dos quais se destacam a avaliação da remodelagem ventricular esquerda, do componente vascular, a avaliação da AVA e do TSVE pelos métodos tridimensionais (tomográficos e não tomográficos), e a determinação do score de cálcio na válvula aórtica.
Os dados apresentados parecem conferir um prognóstico reservado aos doentes com EA paradoxal, embora não seja clara qual a fase evolutiva na história natural da estenose valvular aórtica (modelo A versus B) (Figura 4).
É de assinalar que a maior parte dos estudos assinalados apontem para um melhor prognóstico dos doentes com EA paradoxal quando submetidos a um tratamento de substituição valvular, quando comparados com o tratamento médico. É, portanto, reconhecido nos documentos orientadores sobre doença valvular, europeu e americano, que a EA paradoxal tem uma indicação classe IIa (embora com nível de evidência C) para substituição valvular aórtica, na presença de sintomas. Importa recordar as limitações associadas aos estudos que avaliaram o impacto prognóstico da substituição valvular nos doentes com EA paradoxal e que estão sumariados na Tabela 1, nomeadamente com a seleção dos doentes, com o desenho dos estudos (um único centro, análises retrospetivas, falta de aleatorização) e com a existência de variáveis de confundimento.
ConclusõesO fenótipo de EA paradoxal caracterizado por um baixo volume sistólico de ejeção e baixo gradiente é frequente nos doentes com EA e boa função sistólica do VE. É reconhecido que os erros de medição, as inconsistências da equação da continuidade e o descontrolo tensional podem ser responsáveis por achados contraditórios na avaliação de um doente com EA. Embora a literatura não seja consensual, o prognóstico da EA paradoxal sintomática é desfavorável. No doente com EA paradoxal sintomática, a terapêutica de substituição valvular poderá ser equacionada.
LimitaçõesA presente revisão incluiu apenas artigos aceites para publicação até dezembro de 2014. Assinalamos que a representatividade dos estudos na avaliação da qualidade foi baixa (25% do total de artigos).
ContribuiçõesRC realizou a pesquisa bibliográfica, elaborou a síntese da literatura e redigiu uma primeira versão do manuscrito. RT idealizou a revisão, discutiu ativamente os resultados, modificou o documento inicial para a primeira submissão e elaborou a resposta aos revisores. MJV realizou a avaliação da qualidade dos estudos e teve um papel importante na elaboração da resposta aos revisores. LG participou ativamente na discussão dos resultados e na correção do manuscrito.
Conflito de interessesOs autores declaram não terem nenhum conflito de interesse.


 AVA: área valvular aórtica;
AVA: área valvular aórtica; 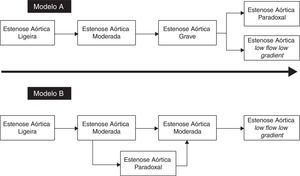
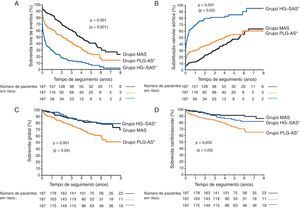 SVAC, sobrevida global e sobrevida cardiovascular. Figura do estudo de Clavel et al.10, publicado com a permissão da Elsevier. Nesta análise é possível observar que, em A, a sobrevida livre de eventos a um e a cinco anos de seguimento foi de 63 e 24%, respetivamente para EA paradoxal, versus 30 e 9%, para a EA grave e alto gradiente, e 85 e 41% para a EA moderada (p<0,01). Em B, é possível constatar que o grupo de doentes com EA paradoxal foi menos referenciado para
SVAC, sobrevida global e sobrevida cardiovascular. Figura do estudo de Clavel et al.10, publicado com a permissão da Elsevier. Nesta análise é possível observar que, em A, a sobrevida livre de eventos a um e a cinco anos de seguimento foi de 63 e 24%, respetivamente para EA paradoxal, versus 30 e 9%, para a EA grave e alto gradiente, e 85 e 41% para a EA moderada (p<0,01). Em B, é possível constatar que o grupo de doentes com EA paradoxal foi menos referenciado para 
