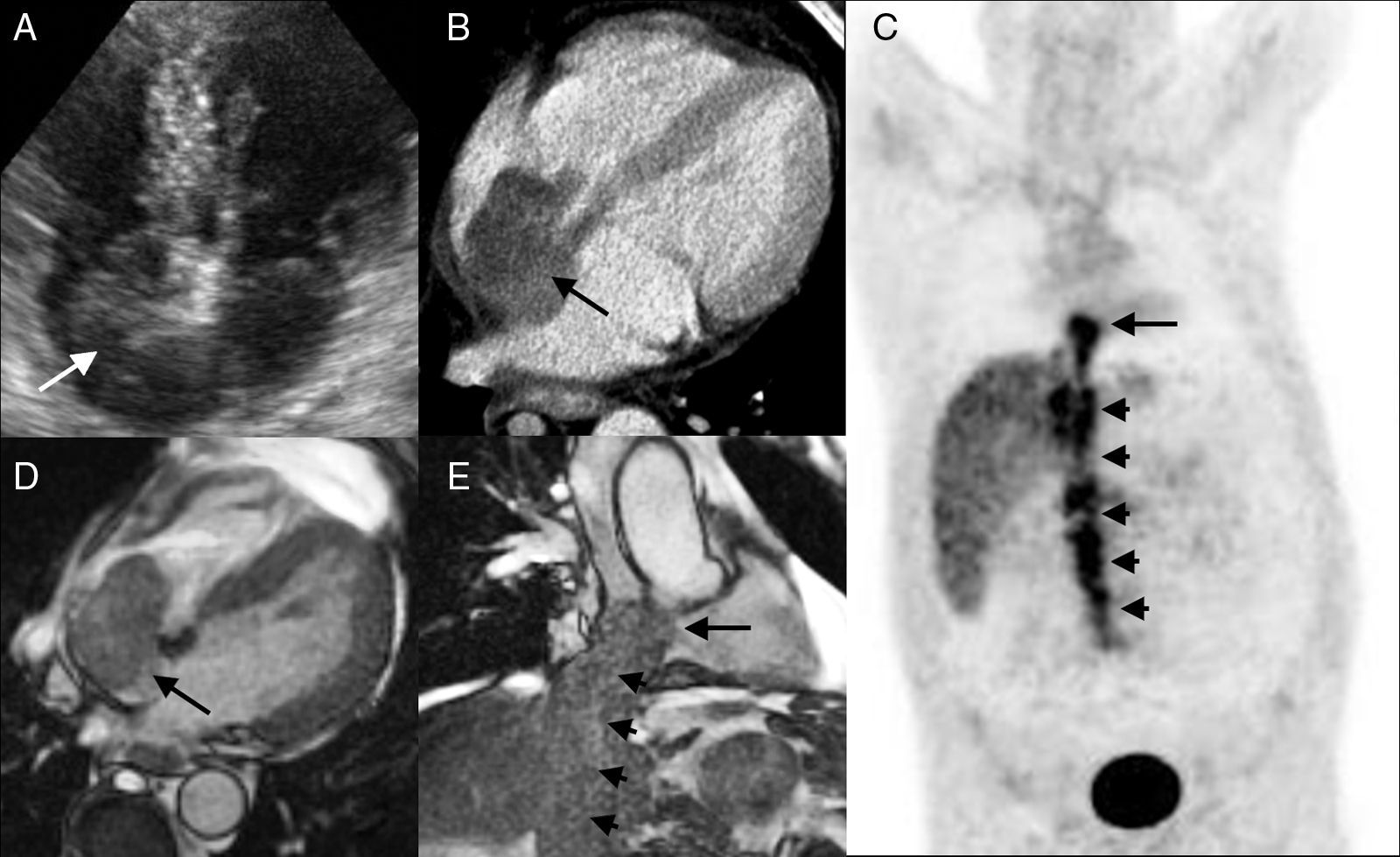
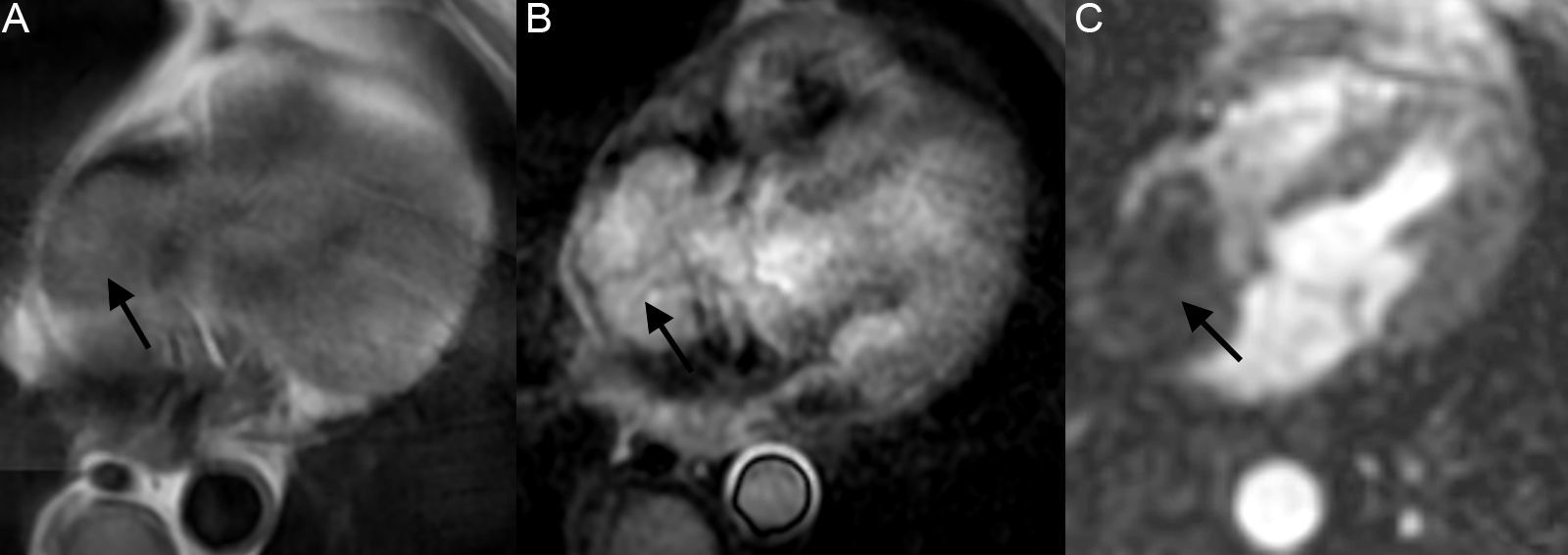
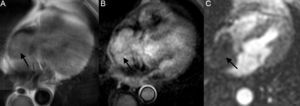
A 65-year-old man with no history of cardiovascular disease was admitted because of abdominal pain, nausea and lower limb edema. At clinical examination he presented hepatomegaly, ascites and laboratory evidence of liver failure. The echocardiogram (Figure 1A) showed preserved biventricular function, but a large irregular mass was visible in the right atrium (arrow; Supplementary data, Movie 1 and 2). Computed tomography (Figure 1B) showed patchy contrast uptake and positron emission tomography (Figure 1C) showed pathological uptake of 18-fluoro-deoxy-glucose in the mass (arrow), extending along the inferior vena cava (arrowheads), suggesting a neoplastic nature. At cardiovascular magnetic resonance (Figure 1D and E; Supplementary data, Movie 3 and 4) the mass involved the right atrium (arrow) and extended into the inferior vena cava (arrowheads); moreover, it presented irregular contours and signal characteristics typical of a neoplastic mass, being irregularly hyperintense in T1-weighted fast-spin-echo imaging (Figure 2A), T2-weighted short-tau inversion recovery fast-spin-echo imaging (Figure 2B) and post-contrast T1-weighted gradient-echo imaging (Figure 2C). Because of his advanced disease and poor clinical condition, the patient did not undergo surgical intervention and died a few days after diagnosis. Autopsy confirmed the mass to be a leiomyosarcoma arising from the inferior vena cava with thrombotic apposition (Figure 3), composed of spindle cells with positive immunohistochemistry staining for smooth muscle actin, desmin and vimentin.
(A) Apical 4-chamber echocardiographic view, showing preserved biventricular function, but a large irregular mass inside the right atrium (arrow); (B) computed tomography, 4-chamber view, showing patchy contrast uptake inside the right atrial mass (arrow); (C) positron emission tomography, coronal view, showing pathological uptake of 18-fluoro-deoxy-glucose in the mass (arrow), extending along the inferior vena cava (arrowheads), suggesting a neoplastic nature with variable retrograde thrombotic apposition; (D and E) cardiovascular magnetic resonance image of the neoplastic mass occupying most of the right atrium (D, 4-chamber cine view) and extending along the inferior vena cava (E, parasagittal cine view).
Magnetic resonance long-axis image of the heart, showing a large mass inside the right atrium (arrow) appearing irregularly hyperintense in a T1-weighted fast-spin-echo sequence (A), a T2-weighted short-tau inversion recovery fast-spin-echo sequence (B) and a post-contrast T1-weighted gradient-echo sequence (C). These signal characteristics, together with the local invasiveness of the mass, indicated a neoplastic nature.
Macroscopic autopsy specimen of the inferior vena cava (after removal of the large intravascular thrombus), showing an irregular tissue mass growing from the vessel wall; immunohistochemistry study identified the growth as a leiomyosarcoma (positive for smooth muscle actin, desmin and vimentin).
Leiomyosarcoma of the inferior vena cava is a rare tumor that presents in an insidious manner with non-specific symptoms. Diagnosis often comes too late and, even in patients who undergo radical surgical resection, prognosis remains extremely poor. Multimodality imaging is crucial for early diagnosis and therapy.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.