Despite diagnostic and therapeutic advances, infective endocarditis (IE) remains a challenging and potentially lethal disease. The prognosis of IE remains poor; in the last 30 years, its incidence and mortality have only been marginally reduced. Early identification of high-risk patients can change the course of the disease and improve outcomes.
Objectives and methodsTo describe and investigate predictors of mortality during hospital stay and in the six months after discharge in a cohort of left-sided IE patients in two tertiary centers. All patients diagnosed with IE (ICD9 code 133) were registered in a uniform database.
ResultsOne hundred and forty-seven consecutive case patients with left-sided IE were included in this study. Thirty-five patients (23.8%) died during hospital stay. The variables significantly associated with increased mortality in univariate analysis were Charlson index ≥5, use of immunosuppressants, sepsis (severe sepsis and/or septic shock), cardiogenic shock and inappropriate use of antibiotic therapy. Conversely, surgical therapy and hospital length of stay ≥30 days were significantly associated with lower mortality. In multivariate analysis the most important predictors of in-hospital mortality were sepsis (severe and/or shock), use of immunosuppressants and inappropriate use of antibiotic therapy. There was a significant relation between the use of immunosuppressants and the occurrence of sepsis. The presence of significant valve disease after IE significantly increased the risk of heart failure.
ConclusionsOur results may help to identify IE patients at increased risk for in-hospital mortality and medium-term disability. These findings can help to identify candidates for earlier and more aggressive management.
Apesar dos avanços no diagnóstico e terapêutica da endocardite infecciosa, esta patologia mantém-se desafiante e potencialmente fatal. O prognóstico desta doença mantevese praticamente inalterado nos últimos 30 anos. A identificação precoce dos doentes de alto risco pode alterar o curso da doença e melhorar o prognóstico.
Objetivos e métodosDescrever e investigar os preditores de mortalidade durante o internamento e nos seis meses após a alta dos doentes com diagnóstico de endocardite infecciosa esquerda (código ICD9: 133).
ResultadosForam incluídos 147 doentes com endocardite infecciosa esquerda. Trinta e cinco doentes (23,8%) morreram durante o internamento. Registou-se um aumento significativo da mortalidade na análise univariada com: Charlson index ≥ 5, uso de imunossupressores, sépsis (sépsis grave e/ou choque sético), choque cardiogénico e uso inapropriado de antibioterapia. Contudo, a realização de cirurgia cardíaca e tempo de internamento ≥ 30 dias associaramse significativamente com taxas de mortalidade mais baixas. Os preditores mais relevantes de mortalidade intra-hospitalar na análise multivariada foram: sépsis (grave e/ou choque), uso de imunossupressores e uso inapropriado de antibioterapia. Verificou-se uma interação significativa entre o uso de imunossupressores e a ocorrência de sépsis. A presença de patologia valvular após resolução do quadro infeccioso aumentou o risco de insuficiência cardíaca.
ConclusõesOs nossos resultados podem ajudar a identificar quais os doentes com maior risco de mortalidade intra-hospitalar e de complicações a médio prazo, assim como ajudar a triar os candidatos que devem ser sujeitos a uma monitorização mais apertada.
Despite diagnostic and therapeutic advances, infective endocarditis (IE) remains a challenging and potentially lethal disease1 with a dismal prognosis. In the last 30 years the incidence and mortality of IE have only been marginally reduced.2 Most series report in-hospital mortality between 9.6 and 26%3–7 and long-term (more than six months) mortality between 20 and 37.1%.7–9 Only a limited number of studies have focused on medium-term outcomes.10
Heterogeneity in clinical presentation, the presence of structural heart disease, the different types of microorganism involved, the development of complications, and patient characteristics, all require a multidisciplinary team to be involved in the treatment of IE.1,11 Many studies suggest that early identification of high-risk patients can change the course of the disease and improve outcomes.12
Prognosis is influenced by four types of factors: patient characteristics, associated complications, microbial etiology, and echocardiographic findings.3,13 Patients with heart failure (HF), perivalvular complications, and/or methicillin-resistant Staphylococcus aureus (MRSA) infections usually have higher mortality and often need surgery in the active disease phase.13,14 Several studies have identified different independent prognostic factors associated with higher mortality, such as higher number of comorbidities, advanced age, renal insufficiency, septic shock, insulin-dependent diabetes, heart failure with reduced ejection fraction, prosthetic valve IE, and cerebral embolism.3,5,7,15,16
ObjectivesTo determine the characteristics of our population with left-sided IE and to investigate factors associated with higher mortality during hospital stay and in the six months after discharge in a two-center cohort of left-sided IE patients. This analysis is intended to identify clinical procedures that could be improved to minimize mortality associated with left-sided IE.
MethodsStudy populationAll patients diagnosed with IE (ICD9 code 133) in two tertiary hospitals in Porto, Portugal, were registered in a uniform database based on information from medical records between January 2000 and June 2011. The study included cases from both community and referral hospitals.
Criteria and definitionsLeft-sided IE was defined according to the modified Duke criteria17 for definite or possible IE.
For each case, data were collected regarding age, gender, valvular involvement, comorbidities, echocardiographic findings, microbiologic agents, associated complications, treatment (including surgery), and outcome (in-hospital and in the six months after discharge). The European System for Cardiac Operative Risk Evaluation (EuroSCORE) surgical risk score18 was determined in all patients. In patients undergoing surgery, the Society of Thoracic Surgeons (STS) surgical risk score19 was also used.
Patients with no signs of infection and negative blood cultures after a complete course of antibiotic therapy were considered cured. Relapse was defined as a new IE episode caused by the same agent within six months. Reinfection was defined as a new IE episode caused by a different agent.
Immunosuppression was considered to be present when patients had been taking immunosuppressants or ≥15 mg of prednisolone or equivalent for more than three months and/or had CD4 counts of <350 cells/mm3 when infected with human immunodeficiency virus.
Appropriacy of antibiotic therapy was defined according to the latest guidelines.12
The primary outcome was overall all-cause in-hospital mortality and death from cardiac cause within six months of discharge.
The study was approved by the local ethics committee.
Statistical analysisComparison between groups was performed with parametric or non-parametric tests, as appropriate. Continuous variables are expressed as mean ± standard deviation (SD) or median (inter-quartile range, IQR). Categorical variables are expressed in absolute numbers and proportions.
The association between variables and the primary outcome was first tested by univariate analysis. A significant association was defined by a p value ≤0.05. Variables with significant association were tested by stepwise multivariate analysis. Predictors of outcome were identified by logistic regression analysis. The statistical analysis was performed using SPSS software version 19, Chicago, IL, USA.
ResultsOne hundred and forty-seven consecutive case patients with left-sided IE were included. The median age was 63 years (IQR 45-74). One hundred and five (71.4%) were male.
One hundred and twenty-nine (87.8%) cases were considered as definite and 18 (12.2%) as possible IE, according to the modified Duke criteria.
Most patients (128, 87.1%) had IE on native valves. Of the 19 (12.9%) patients with prosthetic valves, 3 (16%) were considered early and 16 (84%) late IE. The aortic valve was affected in 74 (50.3%) cases, the mitral valve in 60 (40.8%), and both valves in 13 (8.8%) patients.
Ninety-three patients (63.3%) underwent both transthoracic (TTE) and transesophageal (TEE) echocardiography, 48 (32.7%) had TTE alone, and six (4.1%) TEE alone. Overall, 81 (55.1%) had a valvulopathy and/or intervention possibly predisposing for IE: 31 (21.1%) had degenerative valvular disease; 20 (13.6%) had prosthetic valves; 12 (8.2%) had congenital heart disease; 12 (8.2%) had recently undergone an invasive gastrointestinal intervention; five (3.4%) had previous IE; and one (0.7%) had rheumatic valvular disease.
The median Charlson index was 5 (IQR 3-7). One hundred and sixteen (78.9%) patients had significant comorbidities. Of these, 37 (25.2%) had diabetes (of whom 15 [10.2%] were taking insulin and 22 [15%] were taking oral antidiabetic agents), 27 (18.4%) were taking immunosuppressive agents, 17 (11.6%) had renal failure undergoing dialysis, 15 (10.2%) had active cancer, 15 (10.2%) were intravenous drug abusers, 12 (8.2%) had liver cirrhosis, and 11 (7.5%) had chronic obstructive pulmonary disease (COPD).
Fever and/or general symptoms were present for about a month before admission (median 27.5 days, IQR 15-30).
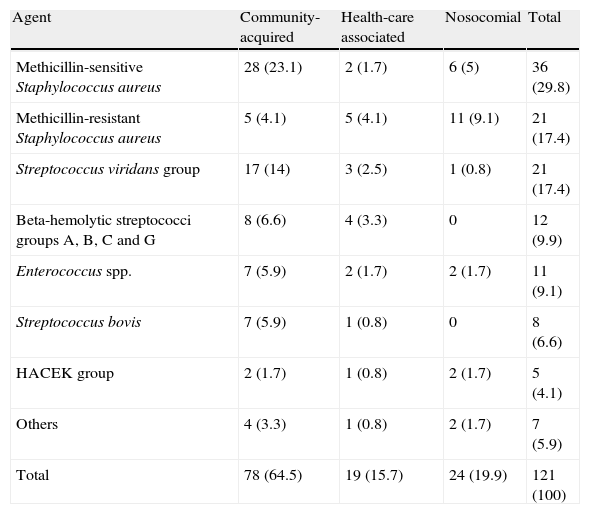
Etiology was established by isolating the causative agent from blood culture in 121 (82.3%) patients. Ninety-eight (66.7%) of the infections were community-acquired, 21 (14.3%) were health-care associated, and 28 (19%) were nosocomial. Methicillin-sensitive Staphylococcus aureus (MSSA) was the most frequent microorganism isolated, followed by methicillin-resistant Staphylococcus aureus (MRSA), Streptococcus viridans group, beta-hemolytic streptococci groups A, B, C and G and Enterococcus spp. (Table 1). Antibiotic therapy was considered appropriate in 123 (83.7%) patients. In the 24 (16.3%) patients in whom antibiotic therapy was considered inappropriate, this was due to short duration of treatment in nine (6.1%) patients, inappropriate spectrum in nine (6.1%) patients, and inappropriate duration and spectrum in four (2.7%). Five (3.4%) patients had infection relapse and another five had reinfection.
Microbiologic etiology by mode of acquisition.
| Agent | Community-acquired | Health-care associated | Nosocomial | Total |
| Methicillin-sensitive Staphylococcus aureus | 28 (23.1) | 2 (1.7) | 6 (5) | 36 (29.8) |
| Methicillin-resistant Staphylococcus aureus | 5 (4.1) | 5 (4.1) | 11 (9.1) | 21 (17.4) |
| Streptococcus viridans group | 17 (14) | 3 (2.5) | 1 (0.8) | 21 (17.4) |
| Beta-hemolytic streptococci groups A, B, C and G | 8 (6.6) | 4 (3.3) | 0 | 12 (9.9) |
| Enterococcus spp. | 7 (5.9) | 2 (1.7) | 2 (1.7) | 11 (9.1) |
| Streptococcus bovis | 7 (5.9) | 1 (0.8) | 0 | 8 (6.6) |
| HACEK group | 2 (1.7) | 1 (0.8) | 2 (1.7) | 5 (4.1) |
| Others | 4 (3.3) | 1 (0.8) | 2 (1.7) | 7 (5.9) |
| Total | 78 (64.5) | 19 (15.7) | 24 (19.9) | 121 (100) |
Data are expressed as number of cases (% of total).
Seventy-nine (53.7%) patients had a single vegetation smaller than 20 mm, 16 (10.9%) had a single vegetation larger than 20 mm, and 52 (35.4%) had multiple vegetations.
Complications were frequent: 54 (36.7%) had severe valvular regurgitation (28 [19%] involving the aortic valve and 26 [17.7%] involving the mitral valve), 39 (26.5%) had perivalvular complications (of whom 27 [18.4%] had an abscess, five [3.4%] had a fistula, five [3.4%] had perforation, two [1.4%] had aneurysm, 50 (34%) had peripheral and/or splenic embolic phenomena, 31 (21.1%) presented neurologic complications (of whom 21 [14.3%] had septic emboli, six [4.1%] had hemorrhage, three [2%] had abscess, and one [0.7%] had meningitis), 22 (15%) had septic shock, 16 (10.9%) had cardiogenic shock, and three (2%) had myocardial infarction.
Valvular surgery was performed in 57 (38.8%) patients (urgent/emergent in 47 [31.9%] patients and scheduled in 10 [6.8%] cases). Of the patients undergoing surgery, the aortic valve was replaced in 28 (19%) patients, the mitral valve in 18 (12.2%), and both valves in 10 (6.8%). All the 57 patients undergoing surgery had heart failure and valve dysfunction. Of these, 40 (70%) had severe valvular regurgitation and 24 (42%) had perivalvular complication with extension of the infectious process. In the patients who underwent surgery, the median STS score was 4.5 (IQR 1.4-8.3), and the median EuroSCORE was 4.4 (IQR 1.6-6.9). There were no differences in EuroSCORE values between patients who did and who did not undergo surgery (OR 0.99; 95% confidence interval [CI] 0.97-1; p=0.9). Of these 57 patients post-surgery information was available for 54: 14 (25.9%) had complications (four [29%] pneumonia, two [14%] arrhythmia, two [14%] stroke, two [14%] death, two [14%] cardiac tamponade, one [7%] ischemic heart disease, and one [7%] valvular dysfunction); the other 40 (74.1%) had no events.
Thirty-five patients (23.8%) died during hospital stay. The main causes of death were septic shock in 13 (37.1%) patients, cardiogenic shock in 8 (22.9%), and neurologic complications in a similar percentage.
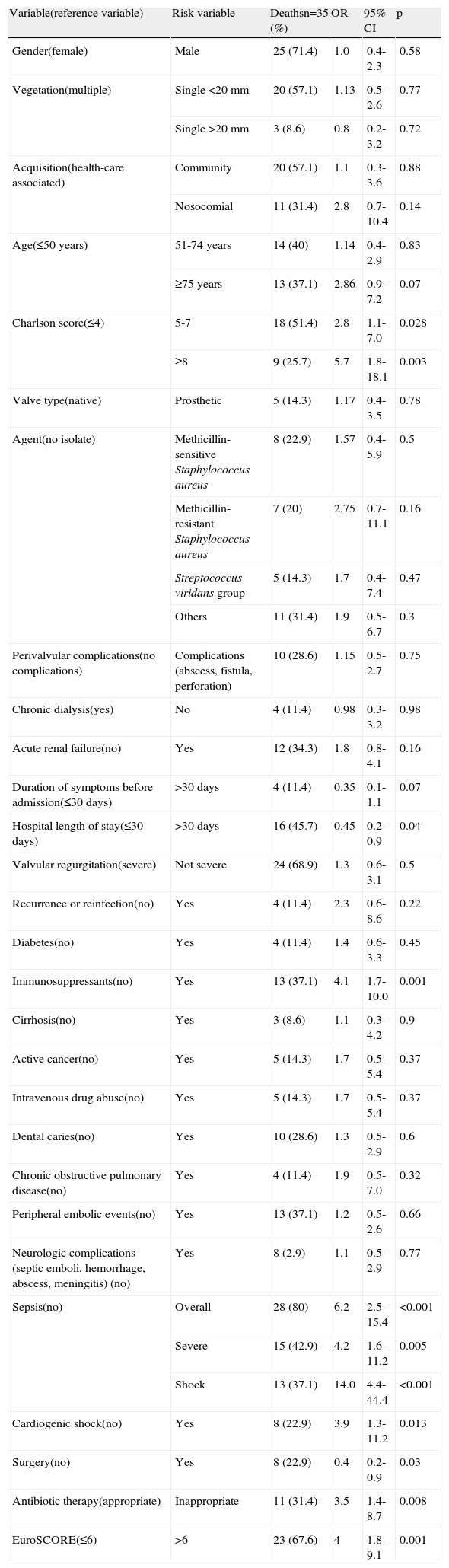
The variables significantly associated with increased in-hospital mortality in univariate analysis were Charlson index ≥5, EuroSCORE >6, use of immunosuppressants, sepsis (severe and/or shock), cardiogenic shock and inappropriate use of antibiotic therapy. Conversely, patients who underwent surgery and those with hospital stay ≥30 days had significantly lower mortality (Table 2). In multivariate analysis the most important predictors of mortality were sepsis (severe and/or shock) (odds ratio [OR] 10.6; 95% CI 3.5-31.7; p<0.001), use of immunosuppressants (OR 8.6; 95% CI 2.6-28.8; p<0.001), EuroSCORE >6 (OR 3.5; 95% CI 1.2-9.7; p=0.019), and inappropriate use of antibiotic therapy (OR 6.8; 95% CI 2.0-23.6; p=0.002). There was a significant relation between the use of immunosuppressants and sepsis (p=0.003).
Univariate analysis of in-hospital mortality.
| Variable(reference variable) | Risk variable | Deathsn=35 (%) | OR | 95% CI | p |
| Gender(female) | Male | 25 (71.4) | 1.0 | 0.4-2.3 | 0.58 |
| Vegetation(multiple) | Single <20 mm | 20 (57.1) | 1.13 | 0.5-2.6 | 0.77 |
| Single >20 mm | 3 (8.6) | 0.8 | 0.2-3.2 | 0.72 | |
| Acquisition(health-care associated) | Community | 20 (57.1) | 1.1 | 0.3-3.6 | 0.88 |
| Nosocomial | 11 (31.4) | 2.8 | 0.7-10.4 | 0.14 | |
| Age(≤50 years) | 51-74 years | 14 (40) | 1.14 | 0.4-2.9 | 0.83 |
| ≥75 years | 13 (37.1) | 2.86 | 0.9-7.2 | 0.07 | |
| Charlson score(≤4) | 5-7 | 18 (51.4) | 2.8 | 1.1-7.0 | 0.028 |
| ≥8 | 9 (25.7) | 5.7 | 1.8-18.1 | 0.003 | |
| Valve type(native) | Prosthetic | 5 (14.3) | 1.17 | 0.4-3.5 | 0.78 |
| Agent(no isolate) | Methicillin-sensitive Staphylococcus aureus | 8 (22.9) | 1.57 | 0.4-5.9 | 0.5 |
| Methicillin-resistant Staphylococcus aureus | 7 (20) | 2.75 | 0.7-11.1 | 0.16 | |
| Streptococcus viridans group | 5 (14.3) | 1.7 | 0.4-7.4 | 0.47 | |
| Others | 11 (31.4) | 1.9 | 0.5-6.7 | 0.3 | |
| Perivalvular complications(no complications) | Complications (abscess, fistula, perforation) | 10 (28.6) | 1.15 | 0.5-2.7 | 0.75 |
| Chronic dialysis(yes) | No | 4 (11.4) | 0.98 | 0.3-3.2 | 0.98 |
| Acute renal failure(no) | Yes | 12 (34.3) | 1.8 | 0.8-4.1 | 0.16 |
| Duration of symptoms before admission(≤30 days) | >30 days | 4 (11.4) | 0.35 | 0.1-1.1 | 0.07 |
| Hospital length of stay(≤30 days) | >30 days | 16 (45.7) | 0.45 | 0.2-0.9 | 0.04 |
| Valvular regurgitation(severe) | Not severe | 24 (68.9) | 1.3 | 0.6-3.1 | 0.5 |
| Recurrence or reinfection(no) | Yes | 4 (11.4) | 2.3 | 0.6-8.6 | 0.22 |
| Diabetes(no) | Yes | 4 (11.4) | 1.4 | 0.6-3.3 | 0.45 |
| Immunosuppressants(no) | Yes | 13 (37.1) | 4.1 | 1.7-10.0 | 0.001 |
| Cirrhosis(no) | Yes | 3 (8.6) | 1.1 | 0.3-4.2 | 0.9 |
| Active cancer(no) | Yes | 5 (14.3) | 1.7 | 0.5-5.4 | 0.37 |
| Intravenous drug abuse(no) | Yes | 5 (14.3) | 1.7 | 0.5-5.4 | 0.37 |
| Dental caries(no) | Yes | 10 (28.6) | 1.3 | 0.5-2.9 | 0.6 |
| Chronic obstructive pulmonary disease(no) | Yes | 4 (11.4) | 1.9 | 0.5-7.0 | 0.32 |
| Peripheral embolic events(no) | Yes | 13 (37.1) | 1.2 | 0.5-2.6 | 0.66 |
| Neurologic complications (septic emboli, hemorrhage, abscess, meningitis) (no) | Yes | 8 (2.9) | 1.1 | 0.5-2.9 | 0.77 |
| Sepsis(no) | Overall | 28 (80) | 6.2 | 2.5-15.4 | <0.001 |
| Severe | 15 (42.9) | 4.2 | 1.6-11.2 | 0.005 | |
| Shock | 13 (37.1) | 14.0 | 4.4-44.4 | <0.001 | |
| Cardiogenic shock(no) | Yes | 8 (22.9) | 3.9 | 1.3-11.2 | 0.013 |
| Surgery(no) | Yes | 8 (22.9) | 0.4 | 0.2-0.9 | 0.03 |
| Antibiotic therapy(appropriate) | Inappropriate | 11 (31.4) | 3.5 | 1.4-8.7 | 0.008 |
| EuroSCORE(≤6) | >6 | 23 (67.6) | 4 | 1.8-9.1 | 0.001 |
CI: confidence interval; OR: odds ratio.
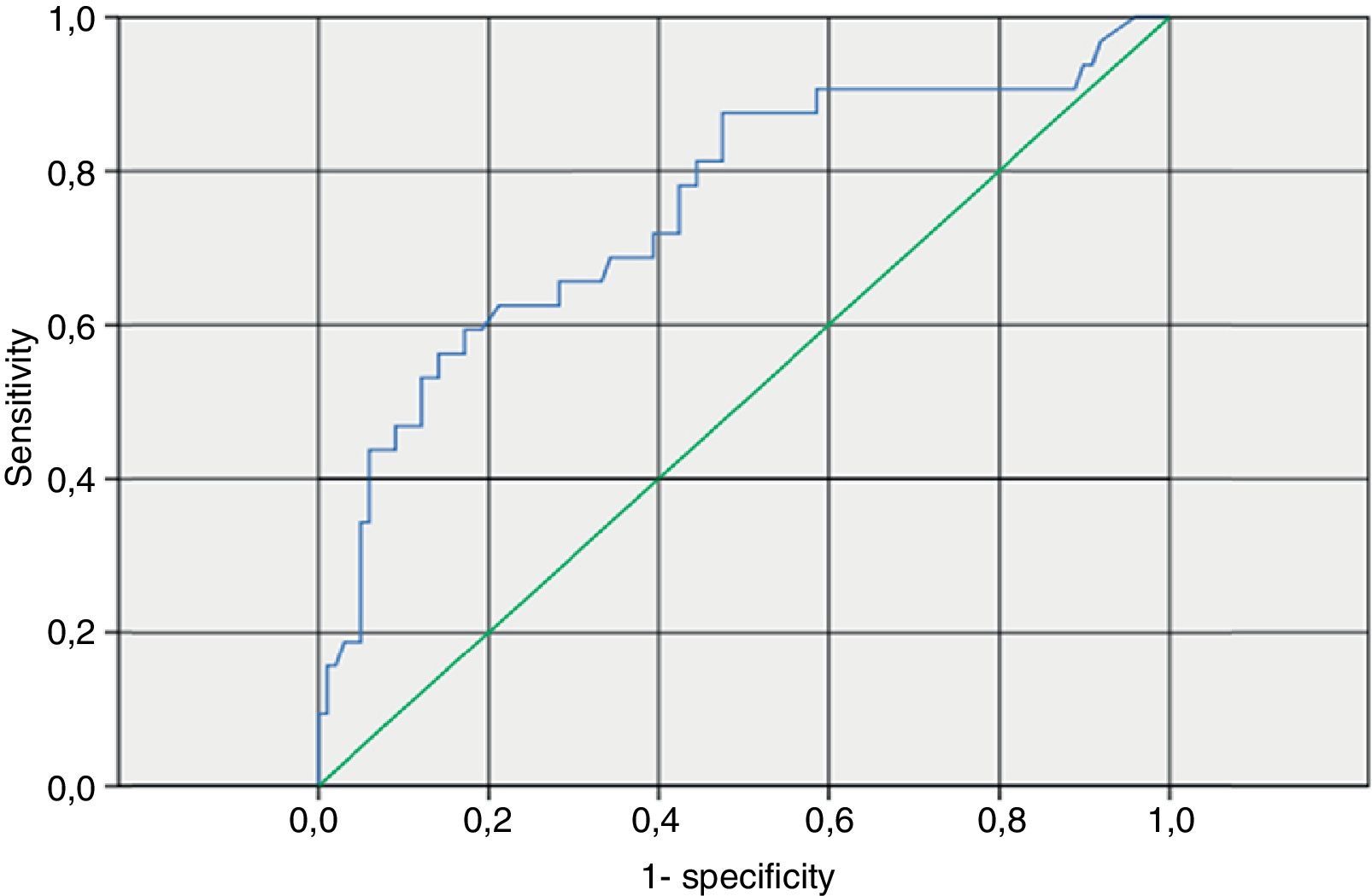
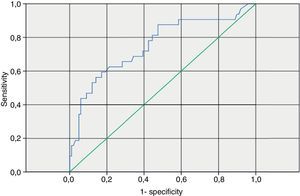
Patients with EuroSCORE >6 had increased mortality, but this was not statistically significant (OR 3; 95% CI 0.6-14.3; p=0.15). In our study the EuroSCORE cut-off that maximized sensitivity and specificity for predicting mortality was 7 (area under the curve 0.75; 95% CI 0.65-0.86; p<0.001) (Figure 1).
The median length of hospital stay was 40 days (IQR 22.5-56).
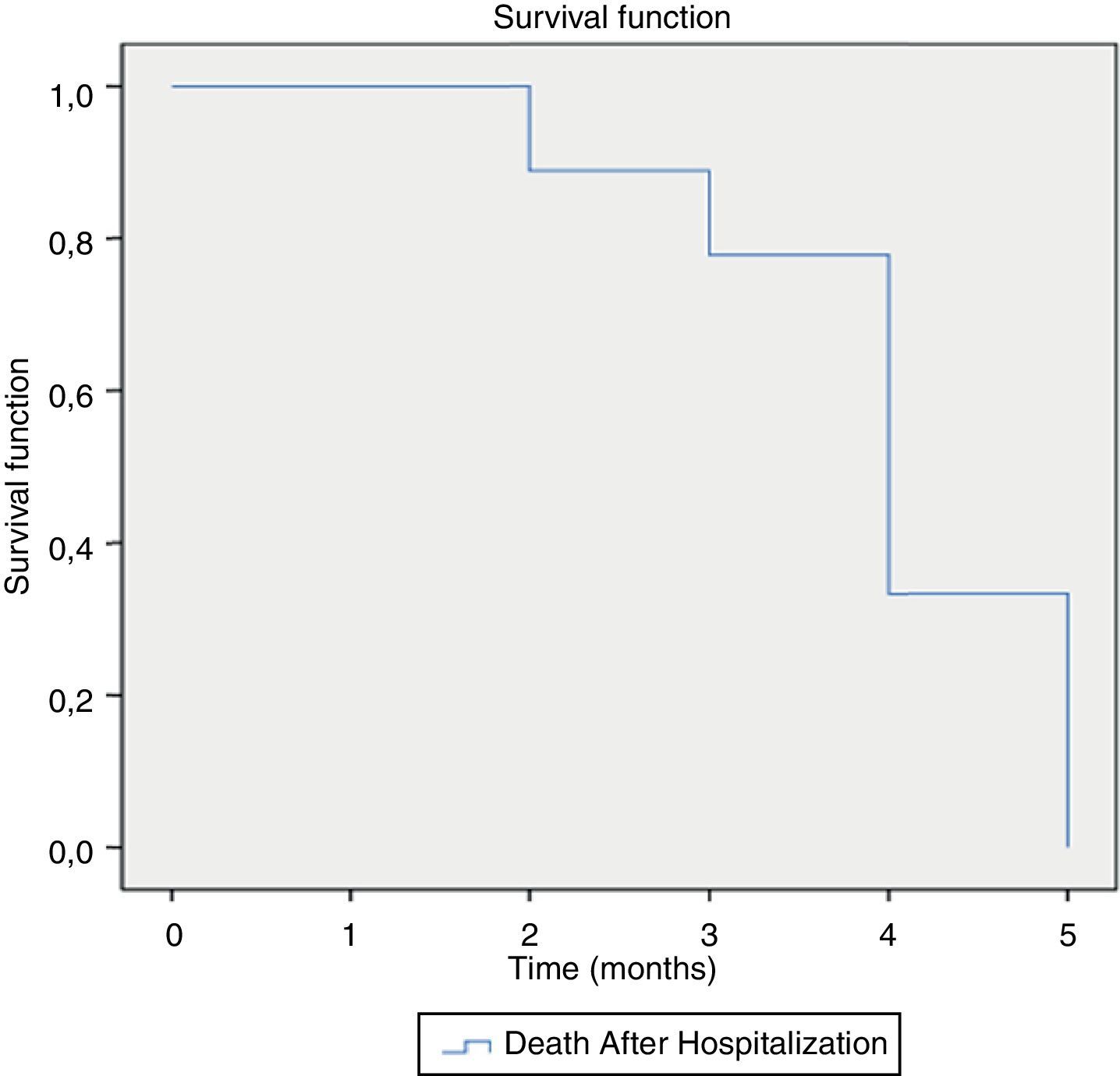
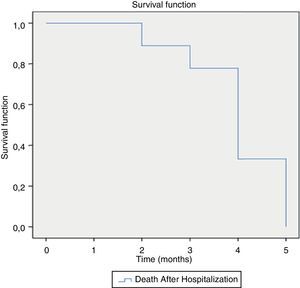
During the six months after hospitalization, another 11 (9.8%) patients died, nine (81.8%) due to IE complications (heart failure due to valvular dysfunction), and two (18.2%) due to other causes (infectious complications). Thirty-eight patients developed heart failure (32 [84.2%] in New York Heart Association [NYHA] class II and six [15.8%] in NYHA class III). Fifteen patients had valvular dysfunction (five [33.3%] moderate aortic regurgitation, one [6.7%] severe aortic regurgitation, seven [46.7%] moderate mitral regurgitation, and two [13.3%] severe mitral regurgitation). Ten patients had neurologic sequelae (six [60%] motor and four [40%] other complications such as epilepsy, diplopia, and aphasia).
The presence of valvular sequelae after IE significantly increased the risk of heart failure and mortality due to cardiac causes during follow-up (OR 7.4; 95% CI 2.3-23.5; p=0.001 and OR 1.6; 95% CI 1.2-6.3; p<0.001, respectively). Mean survival was four months (95% CI 3.3-4.6) (Figure 2).
DiscussionIn our study, we observed similar characteristics and outcomes for IE patients to those described previously.2,10,12
We see in the infrequent use of inappropriate antibiotic therapy (duration and/or spectrum) an opportunity to improve outcome of IE patients.20–22
Delay in diagnosis, complications, length of hospital stay, and mortality remain high in IE.1 Although mortality lower than 20% has been reported,23,24 it usually ranges between 20% and 30%.4 In our study, in-hospital mortality of 23.8% was observed, suggesting that our population reflects similar samples from registries.
A Charlson index of more than 2 has been reported to be an independent risk factor for mortality in previous studies.15,25 We used the age-adjusted index, assuming age to be related to poor prognosis.26 In our study, age ≥75 years had a trend towards higher mortality. Significantly higher mortality was found in patients taking immunosuppressants, similar to that reported in a French study.7
The EuroSCORE tool is used for predicting in-hospital mortality for cardiac surgery.27 A EuroSCORE >6 is considered high risk.28 Our results are consistent with this classification; we also found it useful for predicting overall mortality (in all patients). Based on these findings we recommend calculating the EuroSCORE for any patient admitted for infective endocarditis.
Shorter (≤30 days) hospital stay was associated with increased mortality (most patients died in the first 30 days of hospital stay).
Sepsis with dysfunction of two or more organs was independently associated with increased mortality. Previous studies have found an association between septic shock and increased mortality.5,26 This variable, particularly severe sepsis, helps to identify high-risk patients who can benefit from early, protocol-based aggressive management.
Unlike other studies3 we did not find heart failure at admission (NYHA class III or IV) to be associated with worse prognosis. This observation corroborates previous results pointing in the same direction.26 However, mortality was higher when patients developed cardiogenic shock during hospitalization. One possible explanation for these findings is that development of cardiogenic shock during hospitalization is, in most cases, due to severe valve dysfunction needing emergent surgical repair. By contrast, heart failure at admission (due to fluid overload, arrhythmia, anemia, etc.) can be resolved with medical treatment.
The role of surgery in the treatment of infective endocarditis is expanding, and current guidelines advocate surgical management for complicated left-sided IE.12 Early surgery is also strongly indicated for patients with IE and congestive heart failure.14 Recently, another study found that early surgery in patients with IE and large vegetations significantly reduced death from any cause and specifically embolic events by effectively decreasing the risk of systemic embolism.29 Surgery was also found to be a protective factor in our study. This interesting finding has been described in previous observational studies.3,15,26 This is probably related to the high number of complicated cases with severe valvular dysfunction and cardiogenic shock. However, these results should be interpreted with caution since this was a retrospective observational study.
As expected, inappropriate use of antibiotic therapy was strongly associated with increased mortality, reinforcing the need for correct management of blood cultures, early initiation of antibiotic therapy, and adjustments according to pharmacokinetics, pharmacodynamics, microbiologic findings, and current recommendations regarding length of treatment and potential antimicrobial associations.12
Diabetes,30 prosthetic valve IE,31Staphylococcus aureus etiology,32 neurologic complications,24 large vegetations,25 and perivalvular extension of infection13,24 have all been identified as risk factors for higher mortality. Such associations were not found in our study, possibly due to the small sample size in each setting.
In our study, six-month mortality was 9.8%, similar to medium-term outcomes described by other authors.10,33
Not surprisingly, the presence of valvulopathy after IE significantly increased the risk of heart failure at six months after discharge. No significant associations were found with mortality at six months, possibly due to the small number of deaths recorded.
Our study has certain limitations: (1) it was a retrospective observational study: information was limited to medical records, important data may have been incomplete, and some results may be biased (such as the protective effect of surgery, since high surgical risk patients may have been refused surgery); (2) changes in the clinical management of IE have occurred during the study period; (3) some cases were from referral centers, and so the percentage of complicated cases may be overestimated; (4) some patients were lost to follow-up or transferred to other hospitals.
ConclusionsThe development of severe sepsis is a strong predictor of a dismal outcome and antibiotic treatment should be started promptly. Patients on immunosuppressants also have a worse prognosis. As expected, obtaining an early diagnosis and following the antibiotic guidelines have a positive impact on outcome. The need for surgery is mainly determined by heart failure, which should be carefully evaluated.
Our results may help to identify IE patients at increased risk for in-hospital mortality and medium-term disability. These findings can help to identify candidates for earlier and more aggressive management.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.