Concerns regarding the consequences of ionizing radiation (IR) have been increasing in the field of interventional cardiology (IC). There is little information on reported national and local radiation diagnostic reference levels (DRLs) in catheterization laboratories in Portugal. This study was designed to assess the IR dose exposure during complex percutaneous coronary intervention (PCI), and to set the respective DRLs and future achievable doses (ADs).
MethodsThis was a retrospective cohort study which took place between 2019 and 2020, including patients who underwent complex PCI. Complex PCI was defined as all procedures that encompass treatment of chronic total occlusions (CTO) or left main coronary artery. DRLs were defined as the 75th percentile of the distribution of the median values of air kerma area product (PKA) and cumulative air kerma (Ka,r). ADs were set at the 50th percentile of the study dose distribution. Multivariate analysis was performed using linear regression to identify predictors significantly associated with radiation dose (Ka,r).
ResultsA total of 242 patients were included in the analysis. Most patients underwent a CTO procedure (146, 60.3%). Patients were aged 67.9±11.2 years and mostly male (81.4%). DRLs were set in Ka,r (3012 mGy) and PKA (162 Gy cm2) for complex PCI. ADs were also set in Ka,r (1917 mGy) and PKA (101 Gy cm2). Independent predictors of Ka,r with a positive correlation were PKA (0.893, p<0.001), fluoroscopy time (0.520, p<0.001) and PCI time (0.521, p<0.001).
ConclusionsThis study reports the results of IR in complex PCI. DRLs were set for IR dose exposure measured in Ka,r (3012 mGy) and PKA (162 Gy cm2). ADs, values to be achieved in future assessment, were set to Ka,r (1917 mGy) and PKA (101 Gy cm2).
A preocupação com as consequências da radiação ionizante (IR) aumentou entre a cardiologia de intervenção (IC). Ainda assim, os dados reportados sobre os níveis de referência de dose de radiação (DRLs) são escassos nos laboratórios de hemodinâmica em Portugal. Este estudo foi concebido para aceder às doses de radiação durante a intervenção coronária percutânea complexa (PCI) e para definir os respetivos DRLs e futuras dose a alcançar (ADs).
MétodosEstudo retrospetivo (2019 e 2020) de doentes submetidos a PCI complexa. Definiu-se PCI complexa como os procedimentos que englobaram tratamento de oclusões totais crónicas (CTO) e lesões do tronco comum. Os DRLs são definidos como o percentil 75th da distribuição dos valores medianos do air kerma area product (PKA) e do cumulative air kerma (Ka,r). As ADs foram fixadas no percentil 50th da distribuição da dose de IR do estudo. A análise multivariada foi realizada utilizando a regressão linear para identificar os preditores significativamente associados à dose de radiação (Ka,r).
ResultadosAnálise com 242 doentes. A maioria dos pacientes realizou um procedimento de CTO (146, 60,3%). Os DRLs foram definidos em Ka,r (3012 mGy) e PKA (163 Gy.Cm2) para a PCI complexa. As ADs foram definidas em Ka,r (1917 mGy) e PKA (101 Gy.Cm2). Os preditores independentes de Ka,r com uma correlação positiva foram PKA (0,893, p < 0,001), tempo de fluoroscopia (0,520, p < 0,001) e tempo de PCI (0,521, p < 0,001).
ConclusõesForam definidos em PCI complexa DRLs para exposição à dose de radiação medida em Ka,r (3012 mGy) e PKA (162 Gy.Cm2). As ADs, valores a atingir em futura avaliação, foram definidas em Ka,r (1917 mGy) e PKA (101 Gy.Cm2).
Exposure to ionizing radiation (IR) is a consequence of the improvement in minimally invasive techniques used in interventional cardiology. While this contributes to improved knowledge regarding coronary heart disease (CAD), the introduction of more sophisticated catheters and stents may lead to more complex and time-consuming interventions.1,2
Percutaneous coronary intervention (PCI) is the first line diagnostic and therapeutic method to treat acute coronary syndromes (ACS) and is also an important therapeutic strategy in symptomatic chronic coronary syndromes (CCS). The downside of such procedure is the potentially harmful exposure to IR. The two main biological effects of IR are deterministic (direct effects in tissues like skin burns and cataracts) and stochastic effects (long term carcinogenic alterations), and the risk of radiation-induced cancer increases in direct proportion to effective dose.3–6
Thus, interest in radiation doses in clinical practice has garnered greater interest recently, in particular, the exposure of patients and catheterization laboratory (Cath-Lab) personnel to radiation. Nevertheless, very few Cath-Labs communicate their patients’ IR exposure data.7–10
Diagnostic reference levels (DRLs) are an essential tool to promote optimization in IC procedures, highlighted by the European Commission Basic Safety Standard.11,12 Air kerma area product (PKA) and cumulative air kerma at patient entrance reference points (Ka,r) are the dose descriptors used to calculate DRLs, which are key to defining which levels may lead to harmful consequences.11,13
Diagnostic reference levels should be set and regularly updated at local (hospital) and national levels by the competent national health authority. Fourteen years ago, the SENTINEL project and more recently, the European Commission for Radiation Protection (EUCLID) suggested DRLs in interventional cardiology. There have also been some recent DRLs studies focusing on coronary angiography (CA) and PCI, however, for complex procedures such as the treatment of coronary chronic total occlusions (CTO), left main coronary artery (LMCA) or structural interventions, information on DRLs remain scarce.2,11,14,15
The goal of this study was to establish, for the first time, local (hospital) DRLs for complex PCI procedures, encouraging other Cath-Labs to establish their own, thus contributing to setting national DRLs.
ObjectivesThe study aimed to access the IR dose exposure during complex percutaneous coronary intervention (PCI), and to set the respective DRLs (primary outcome) and future achievable doses (ADs) (secondary outcome).
MethodsThis was a single center retrospective cohort study, taking place between 2019 and 2020, involving patients who underwent complex PCI at a local hospital in Portugal.
Patient selectionComplex PCI was defined as all procedures that encompass treatment of CTO or LMCA. Patients were eligible for the study if they had been diagnosed with an ACS or CCS, in which significant atherosclerotic (vessel stenosis 100% in CTO or ≥50% in LMCA) eligible for angioplasty treatment had been found. CTO was defined as total occlusion of the vessel with an evolution of more than three months. The study recruited adult patients with a body mass index 18.5 to 25 kg/m2 or a weight of 70±15 kg when height was not available for each IR procedure. Patients who only underwent a diagnostic study (CA), despite having CTO or LMCA disease criteria, were excluded from the study. Unsuccessful procedures were also excluded. Baseline patient demographic data, cardiovascular risk factors, clinical, laboratory, echocardiographic and angiographic data were recorded.
The study abided by the principles of the 1975 Declaration of Helsinki and ethical approval was received from the local ethics committee.
Radiation dose measuresThe primary outcome for the study was to set the DRLs by measuring two parameters (PKA in Gy cm2 and Ka,r in mGy) in CTO and LMCA procedures individually, as well as in complex PCI. Both variables summarize the radiation data for fluoroscopy and cineangiography. Data was collected in Siemens Artis Zee equipment (model (240)07716900 of 2017), with respective calibration and validation updated by the manufacturer. DRLs are defined as the 75th percentile (third quartile) of the distribution of the median values of PKA and Ka,r.12,13
The secondary outcome was to calculate achievable doses (ADs), set at approximately the 50th percentile of the study dose distribution. ADs refer to doses to be achieved in future assessments in order to encourage Cath-Labs to reduce exposure and ensure patient protection.16 Additionally, we specifically aimed to identify independent predictors significantly associated with radiation dose and evaluate fluoroscopy and PCI time between procedures.
Statistical analysisCategorical variables are presented as frequencies and percentages, and continuous variables as means and standard deviations, or medians and interquartile ranges for variables with skewed distribution or a significant Shapiro–Wilk test. Comparison between groups was performed using the Chi-square, Student's t-test or Mann–Whitney, as appropriate. Multivariate analysis was performed using linear regression to identify predictors significantly associated with radiation dose (Ka,r). Pearson's and Spearman's correlation coefficient were used to assess the correlation between Ka,r and angiographic variables. p value <0.05 indicates statistical significance. Statistical analysis was performed using IBM SPSS Statistics (IBM SPSS, Chicago, IL, USA, version 21.0).
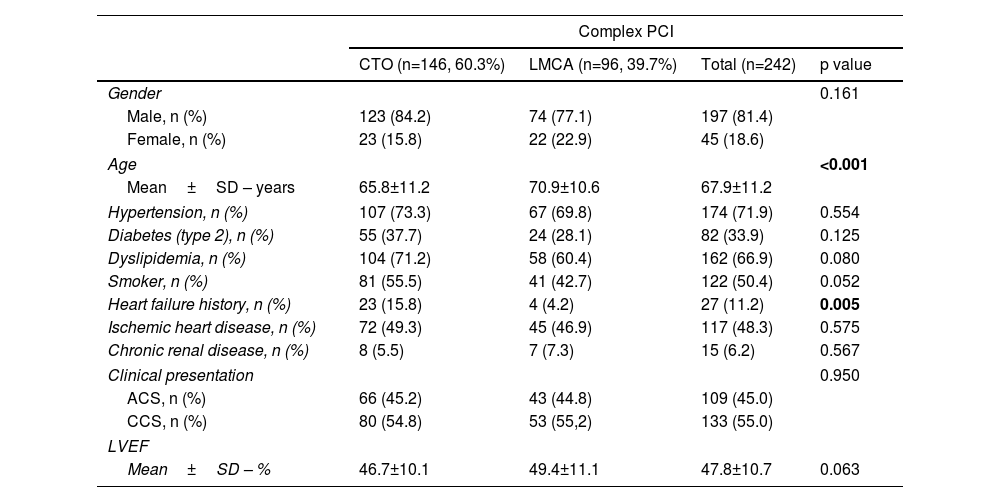
ResultsPatient clinical, echocardiographic, and angiographic characteristicsThe study included data pertaining to a total of 242 patients in the period between 2019 and 2020. Patient demographics are summarized in Table 1. Most patients underwent a CTO procedure (146, 60.3%). On average, patients were aged 67.9±11.2 years, with differences in age noted between procedures (LMCA 70.9±10.6, p<0.001). The male gender was more prevalent (81.4%). Past medical history of hypertension was reported in 71.9% of patients, dyslipidemia in 66.9%, type 2 diabetes in 33.9% and 50.4% were smokers. A previous history of heart failure was more common in the CTO group (15.8%, p=0.005). Ischemic heart disease was present in 48.3% of patients, and 55% were admitted due to chronic coronary syndromes. Left ventricular ejection fraction was mildly reduced overall (47.8±10.7%).
Baseline characteristics of patients submitted to complex PCI, compared by type of procedure (CTO or LMCA).
| Complex PCI | ||||
|---|---|---|---|---|
| CTO (n=146, 60.3%) | LMCA (n=96, 39.7%) | Total (n=242) | p value | |
| Gender | 0.161 | |||
| Male, n (%) | 123 (84.2) | 74 (77.1) | 197 (81.4) | |
| Female, n (%) | 23 (15.8) | 22 (22.9) | 45 (18.6) | |
| Age | <0.001 | |||
| Mean±SD – years | 65.8±11.2 | 70.9±10.6 | 67.9±11.2 | |
| Hypertension, n (%) | 107 (73.3) | 67 (69.8) | 174 (71.9) | 0.554 |
| Diabetes (type 2), n (%) | 55 (37.7) | 24 (28.1) | 82 (33.9) | 0.125 |
| Dyslipidemia, n (%) | 104 (71.2) | 58 (60.4) | 162 (66.9) | 0.080 |
| Smoker, n (%) | 81 (55.5) | 41 (42.7) | 122 (50.4) | 0.052 |
| Heart failure history, n (%) | 23 (15.8) | 4 (4.2) | 27 (11.2) | 0.005 |
| Ischemic heart disease, n (%) | 72 (49.3) | 45 (46.9) | 117 (48.3) | 0.575 |
| Chronic renal disease, n (%) | 8 (5.5) | 7 (7.3) | 15 (6.2) | 0.567 |
| Clinical presentation | 0.950 | |||
| ACS, n (%) | 66 (45.2) | 43 (44.8) | 109 (45.0) | |
| CCS, n (%) | 80 (54.8) | 53 (55,2) | 133 (55.0) | |
| LVEF | ||||
| Mean±SD – % | 46.7±10.1 | 49.4±11.1 | 47.8±10.7 | 0.063 |
CTO: chronic total occlusion; IQR: interquartile range; LMCA: left main coronary artery; LVEF: left ventricular ejection fraction; PCI: percutaneous coronary intervention; SD: standard deviation.
Bold values are statistically significant.
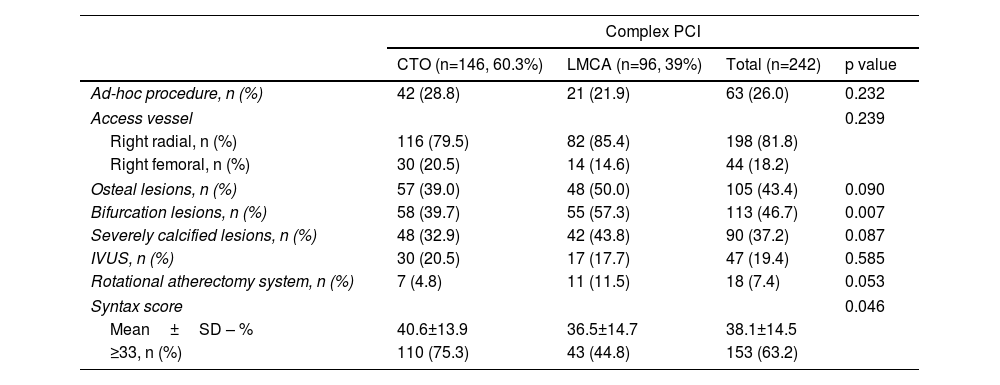
PCI was performed by right radial artery in 198 (81.8%) and non-programmed (ad-hoc) procedure in 63 (26%) patients. Osteal and bifurcations lesions were present in 43.4% and 46.7% of patients, respectively. Syntax score ≥33 was found in 63.2% of patients, mainly in CTO group (75.3% vs. 44.8% in LMCA, p=0.046), and in programmed (post-hoc) interventions (65.4% vs. 57.1% in ad-hoc, p=0.245). Angiographic findings are summarized in Table 2.
Angiographic characteristics of patients submitted to complex PCI, compared by type of procedure (CTO or LMCA).
| Complex PCI | ||||
|---|---|---|---|---|
| CTO (n=146, 60.3%) | LMCA (n=96, 39%) | Total (n=242) | p value | |
| Ad-hoc procedure, n (%) | 42 (28.8) | 21 (21.9) | 63 (26.0) | 0.232 |
| Access vessel | 0.239 | |||
| Right radial, n (%) | 116 (79.5) | 82 (85.4) | 198 (81.8) | |
| Right femoral, n (%) | 30 (20.5) | 14 (14.6) | 44 (18.2) | |
| Osteal lesions, n (%) | 57 (39.0) | 48 (50.0) | 105 (43.4) | 0.090 |
| Bifurcation lesions, n (%) | 58 (39.7) | 55 (57.3) | 113 (46.7) | 0.007 |
| Severely calcified lesions, n (%) | 48 (32.9) | 42 (43.8) | 90 (37.2) | 0.087 |
| IVUS, n (%) | 30 (20.5) | 17 (17.7) | 47 (19.4) | 0.585 |
| Rotational atherectomy system, n (%) | 7 (4.8) | 11 (11.5) | 18 (7.4) | 0.053 |
| Syntax score | 0.046 | |||
| Mean±SD – % | 40.6±13.9 | 36.5±14.7 | 38.1±14.5 | |
| ≥33, n (%) | 110 (75.3) | 43 (44.8) | 153 (63.2) | |
CTO: chronic total occlusion; IVUS: intravascular ultrasound; LMCA: left main coronary artery; SD: standard deviation.
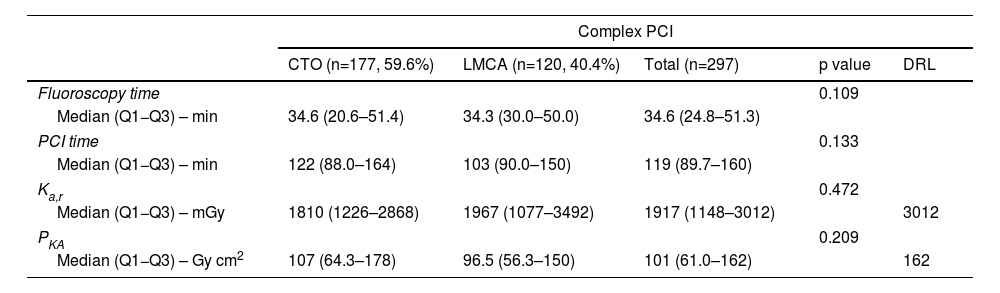
Complex PCI lasted, on average, 119 minutes (min) whereas fluoroscopy took 34.6 min, with no statistical difference found between groups (Table 3).
Radiation dose exposure, DRLs and additional angiographic characteristics of patients submitted to complex PCI, compared by type of procedure (CTO or LMCA).
| Complex PCI | |||||
|---|---|---|---|---|---|
| CTO (n=177, 59.6%) | LMCA (n=120, 40.4%) | Total (n=297) | p value | DRL | |
| Fluoroscopy time | 0.109 | ||||
| Median (Q1−Q3) – min | 34.6 (20.6–51.4) | 34.3 (30.0–50.0) | 34.6 (24.8–51.3) | ||
| PCI time | 0.133 | ||||
| Median (Q1−Q3) – min | 122 (88.0–164) | 103 (90.0–150) | 119 (89.7–160) | ||
| Ka,r | 0.472 | ||||
| Median (Q1−Q3) – mGy | 1810 (1226–2868) | 1967 (1077–3492) | 1917 (1148–3012) | 3012 | |
| PKA | 0.209 | ||||
| Median (Q1−Q3) – Gy cm2 | 107 (64.3–178) | 96.5 (56.3–150) | 101 (61.0–162) | 162 | |
CTO: chronic total occlusion; DRL: diagnostic reference level; Kar: air kerma at patient entrance reference point; LMCA: left main coronary artery; PCI: percutaneous coronary intervention; PKA: air kerma area product.
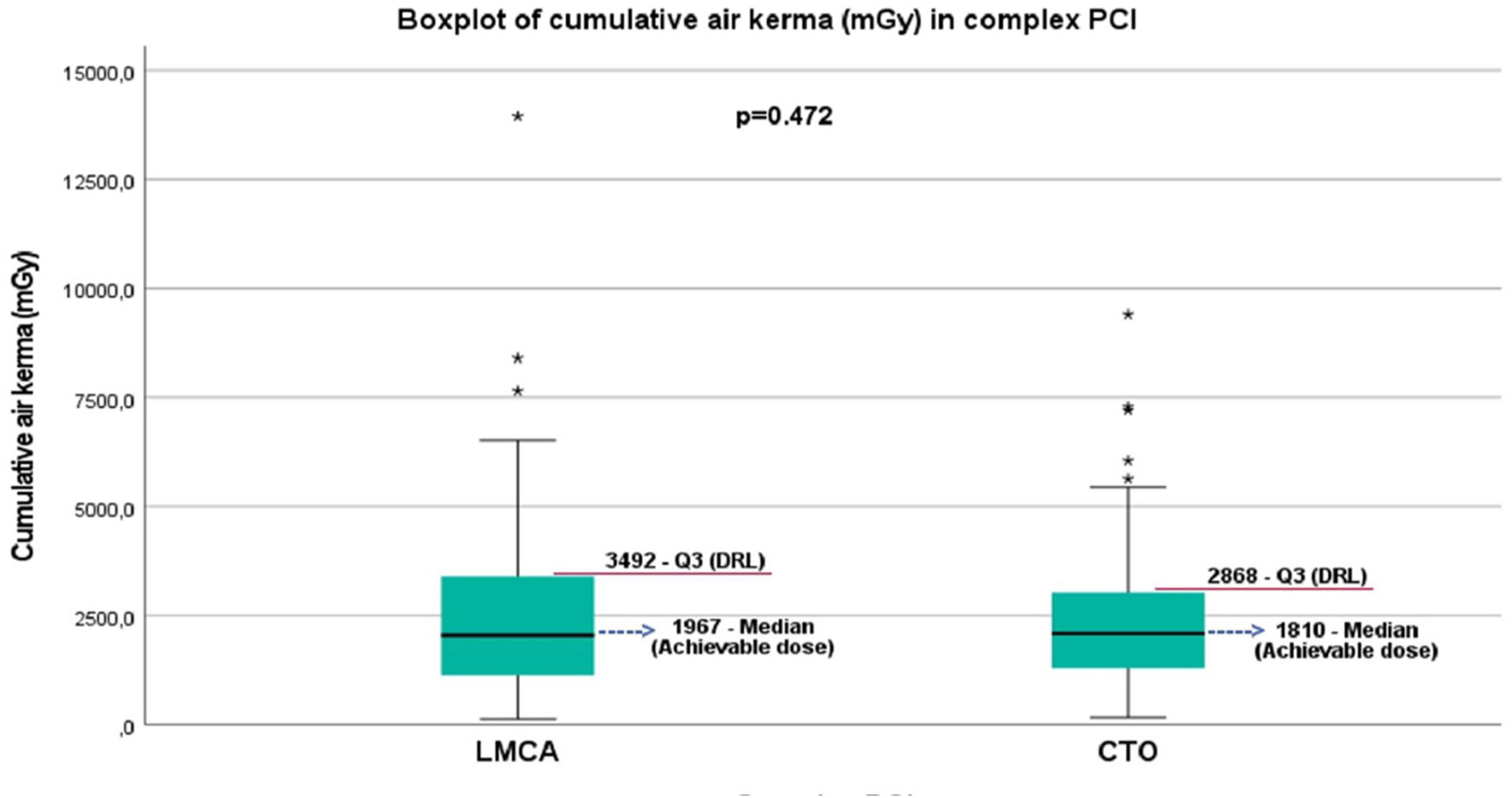
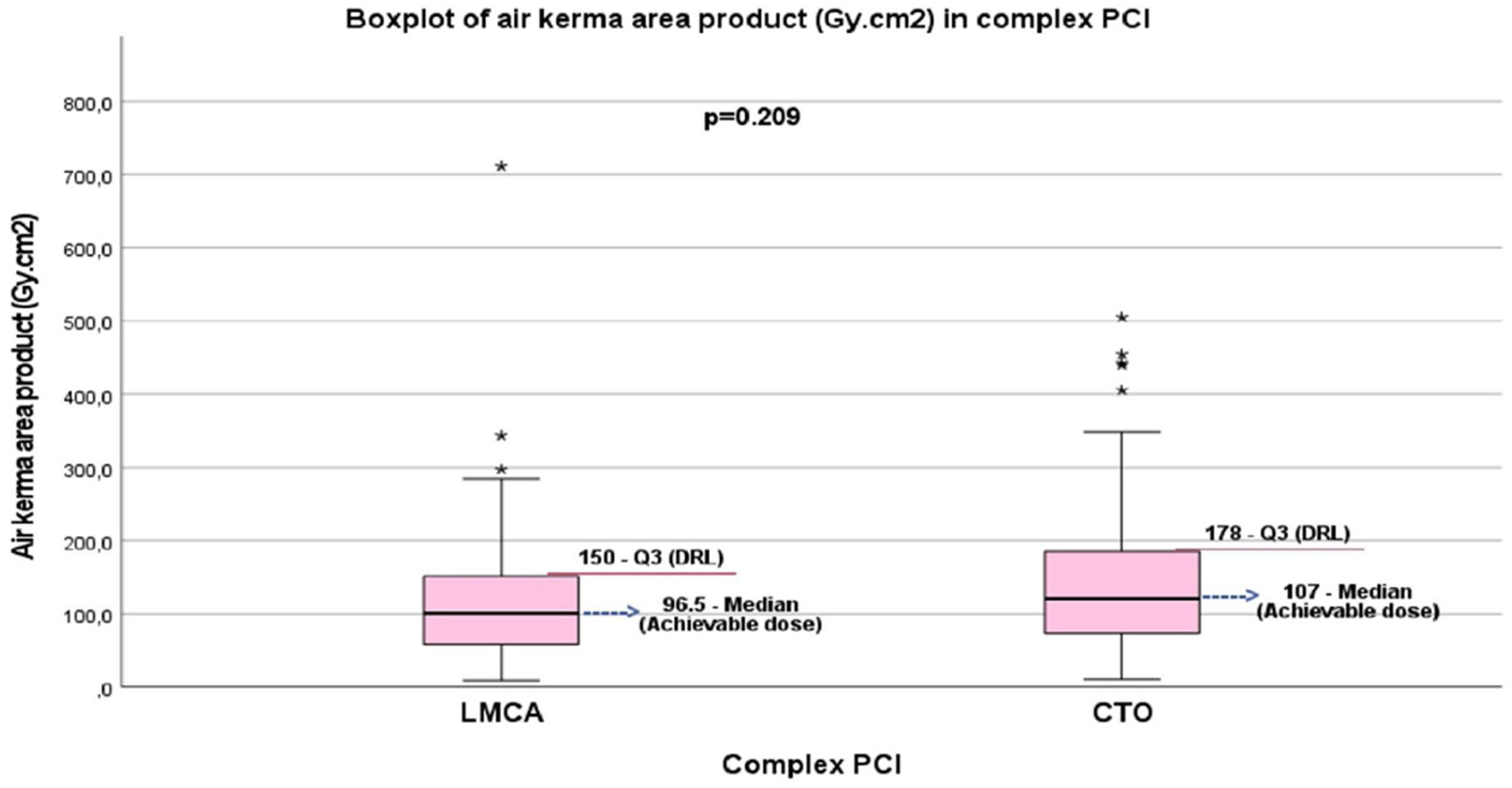
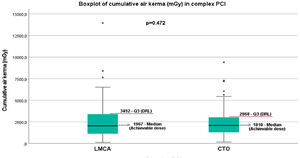
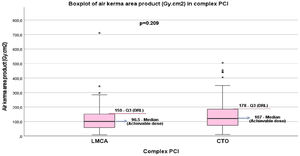
IR exposure measured in PKA and Ka,r was similar, with no statistical difference found between groups. DRLs and ADs of CTO and LMCA procedures were calculated in PKA (CTO DRL 178 Gy cm2; CTO AD 107 Gy cm2) (LMCA DRL 150 Gy cm2; LMCA AD 96.5 Gy cm2) and in Ka,r (CTO DRL 2868 mGy; CTO AD 1810 mGy) (LMCA DRL 3492 mGy; LMCA AD 1967 mGy) (Figures 1 and 2).
Boxplot of cumulative air kerma (mGy) in complex PCI (LMCA vs. CTO treated patients). The figure shows median (black middle horizontal line) that correspond to the achievable dose, IQR (box), 3rd quartile (Q3, red horizontal line) that correspond to DRL and the range of non-outlying data points (lower whisker: lowest data point within the 25th percentile minus 1.5 times IQR; upper whisker: highest data point within the 75th percentile plus 1.5 times IQR). CTO: chronic total occlusion; DRL: diagnostic reference level; IQR: interquartile range; LMCA: left main coronary artery; PCI: percutaneous coronary intervention; *: outliers.
Boxplot of air kerma area product (Gy cm2) in complex PCI (LMCA vs. CTO treated patients). The figure shows median (black middle horizontal line) that correspond to achievable dose, IQR (box), 3rd quartile (Q3, red horizontal line) that correspond to DRL and the range of non-outlying data points (lower whisker: lowest data point within the 25th percentile minus 1.5 times IQR; upper whisker: highest data point within the 75th percentile plus 1.5 times IQR). CTO: chronic total occlusion; DRL: diagnostic reference level; IQR: interquartile range; LMCA: left main coronary artery; PCI: percutaneous coronary intervention; *: outliers.
DRLs of complex PCI were set as defined earlier, with PKA 162 Gy cm2 and Ka,r 3012 mGy (Table 2). ADs, values to be achieved in the next assessment, were set in Ka,r (1917 mGy) and PKA (101 Gy cm2).
When comparing IR exposure measured in Ka,r and PKA between genders, males had higher rates of Ka,r (2543 mGy vs. 1870 mGy in females, p=0.071) and PKA (137 Gy cm2 vs. 91.5 Gy cm2 in females, p<0.001). More complex anatomy (Syntax score ≥33) revealed higher IR exposure (Ka,r 2277 mGy vs. Ka,r 2175 mGy in Syntax score <33, p=0.711), although without statistical significance. Vascular access route, as well as the form of intervention (unscheduled (ad-hoc) vs. programmed (post-hoc)) were also compared, and although vascular access had no influence on the measured IR exposure doses (radial artery median Ka,r 1904 mGy, femoral artery median Ka,r 1969 mGy, p=0.954) (radial artery median PKA 101 Gy cm2, femoral artery median PKA 91.8 Gy cm2, p=0.436), ad-hoc interventions presented significantly lower IR exposure when compared with post-hoc regimes (ad-hoc procedure median Ka,r 1367 mGy, post-hoc procedure median Ka,r 2043 mGy, p=0.002) (ad-hoc procedure median PKA 71.7 Gy cm2, post-hoc procedure median PKA 109 Gy cm2, p<0.001).
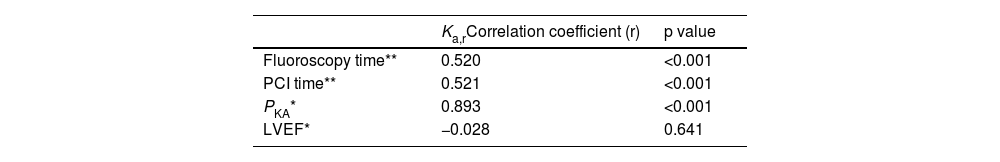
Independent predictors for radiation dose exposure in complex PCIContinuous variables were included in multivariate linear regression analysis. The goal was to identify variables correlated to radiation exposure measured in Ka,r. PKA demonstrated a strong positive correlation with Ka,r (r=0.893, p<0.001), whereas fluoroscopy time (r=0.520, p<0.001) and PCI time both showing moderate positive correlations (Table 4).
Independent predictors for cumulative air kerma exposure in complex PCI (linear regression – correlation between Ka,r and angiographic variable).
| Ka,rCorrelation coefficient (r) | p value | |
|---|---|---|
| Fluoroscopy time** | 0.520 | <0.001 |
| PCI time** | 0.521 | <0.001 |
| PKA* | 0.893 | <0.001 |
| LVEF* | −0.028 | 0.641 |
Kar: air kerma at patient entrance reference point; LVEF: left ventricular ejection fraction; PCI: percutaneous coronary intervention; PKA: air kerma area product.
The technological evolution in IC allowed for a more generalist approach to CAD, not only for diagnostic purposes, but also in therapeutic procedures for more complex coronary disease. Therefore, procedures have become more time-consuming and thus increasingly subjected to IR. For this reason, professionals are becoming more aware of the adverse effects of radiation, and safer techniques and equipment are needed to minimize radiation exposure. The focus on complex disease and PCI should not, therefore, compromise the safety methods used to reduce exposure. Cath-Lab IR dose exposure data during clinical practice are scarce, and evidence from large radiation dose surveys is missing in the literature.2,4,7
As previously defined, complex PCI encompassed patients undergoing CTO or LMCA. Male gender was associated with significantly higher radiation exposure measured by PKA and Ka,r. This finding corroborates that of the PROTECTION VIII study, but reasons for this remain unclear. One plausible explanation in the present study was the higher body surface area and an expected IR dose exposure.7,17,18
The characteristics of CTO lesions and the complexity of the technical procedures makes this intervention more time-consuming and requiring greater image optimization (thus, higher rates of radiation time and contrast doses used). In the present study, CTO and LMCA PCI and fluoroscopy time were not statistically different and CTO had similar procedure times compared to other European and international CTO registries.19–21 Interestingly, a more time-consuming procedure in CTO group was not related to significantly higher IR dose exposure measured in Ka,r and PKA. The CTO group had also more ad-hoc procedures, which are associated with greater PKA radiation exposure in European registries.2 In our analysis, ad-hoc regimes showed statistically significant lower rates of IR exposure, probably associated with less severe CAD, although without statistical significance (57.1% vs. 65.4%, p=0.245). IR exposure was not associated with the complexity of CAD, probably due to the complex anatomy in the entire sample.
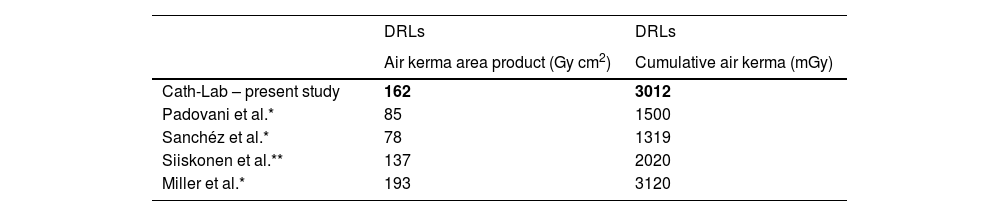
Diagnostic radiation levels help identifying those facilities that are using unusual high IR exposure doses, and are a relevant tool for optimization in IC.11,16,22 As mentioned above, the DRLs were calculated based on the third quartile of the median for the defined IR doses (Ka,r and PKA).13 There is very little international data on DRLs for complex PCI. European registries reflect DRLs for CA, PCI and both procedures. The IR dose exposure and DRLs presented in international registries (Table 5) were significantly lower than those presented in the current study, which can be explained by scarce complex procedures data.7,11,15,23,24 The European register of Siiskonen et al. showed IR dose and respective DRLs according to the type of interventional cardiology procedure. The data reported for complex PCI were specific for CTO procedures, and albeit scarce, were closer to the DRLs presented in the current study. In international CTO registries, the IR dose exposure was also similar to those presented.2,20,21 Miller et al.,25 in a North American register, presented DRLs superior to European data and similar to those in this study, and argue that complex procedures were probably the main reason for the differences reported (Table 4).11
The DRLs reported in the present study and in international registries.
| DRLs | DRLs | |
|---|---|---|
| Air kerma area product (Gy cm2) | Cumulative air kerma (mGy) | |
| Cath-Lab – present study | 162 | 3012 |
| Padovani et al.* | 85 | 1500 |
| Sanchéz et al.* | 78 | 1319 |
| Siiskonen et al.** | 137 | 2020 |
| Miller et al.* | 193 | 3120 |
Cath-Lab: catheterization laboratory of the study; DRLs: diagnostic reference levels.
Bold values are the results from our lab.
To emphasize the “as low as reasonably achievable” (ALARA) principle, optimization of DRLs is encouraged by using the ADs. ADs are set at approximately the 50th percentile (median) of the study dose distribution. In the present study, ADs were set and should supplant DRLs in future assessments.16
Our multivariate analysis showed that independent predictors of IR dose exposure with positive correlation was demonstrated between Ka,r and PKA, Ka,r and fluoroscopy time and Ka,r and PCI time, which corroborates the results from international registries.2,7,11,23
Cath-Labs IR safety performance should be critically reviewed, and safety methods to minimize IR exposure should be implemented. These results are an opportunity for improvement in radiation safety quality practice.
The participation of institutions in IR dose exposure surveys are important, because it will enable the setting of national DRLs to improve radiation “best practice” in Cath-Labs and consequently ensure safer procedures for patients and laboratory personnel. Cath-Lab certification in IR should also become a reality, helping doctors and patients to select safer centers with low IR dose exposure.
ConclusionsThis study reports the results of IR in complex PCI. DRLs were set for IR dose exposure measured in Ka,r (3012 mGy) and PKA (162 Gy cm2). DRLs in the study were relatively higher than the DRLs reported in international registries, but data from complex PCI in these registries are scarce. ADs were set in Ka,r (1917 mGy) and PKA (101 Gy cm2) and DRLs should be updated taking these results into account. National surveys should be a reality, and probably will allow the implementation of new safety methods to minimize IR exposure.
LimitationsSome limitations must be acknowledged. This was an observational study, therefore collected data are limited to medical records. Our sample included only successful CTO or LMCA PCI. Unsuccessful CTO or LMCA PCI was not address and may limit the validity of the results. Also, defining complex PCI as CTO or LMCA was simplistic and an important limitation. Finally, the data in our study are from only one PCI center (composed of 1 Cath-Lab room) with a small sample, so our conclusions may not be generalizable to other cardiac centers.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors would like to express their gratitude to all colleagues who assisted by providing data for this analysis, and their commitment to attenuate the effects of IR in Cath-Labs.