Regular physical exercise is responsible for various health benefits, and is recommended for primary and secondary cardiovascular (CV) prevention. Despite these recognized benefits, various clinical events can occur in athletes, including acute myocardial infarction and sudden cardiac death (SCD); the main cause of SCD in veteran athletes is coronary artery disease (CAD). The relationship between intense exercise training and CAD is controversial, and a U-shaped association has been hypothesized. If this is the case, screening for subclinical CAD in older athletes may be justified, and various different methodologies have been proposed. However, the methodology for screening veteran athletes is not consensual, and several markers of CAD, in addition to clinical CV risk factors, could improve risk stratification in this population. In the present paper we review the published data on CAD in athletes, focusing on the relationship between the dose of exercise and CAD, as well as the implications for pre-participation screening of veteran athletes.
O exercício físico associa-se a múltiplos benefícios para a saúde, estando recomendado na prevenção cardiovascular (CV) primária e secundária. Apesar dos benefícios comprovados, diversos eventos clínicos podem ocorrer em atletas, incluindo enfarte agudo do miocárdio e morte súbita, nos atletas veteranos maioritariamente devido a doença das artérias coronárias (DAC). A relação entre exercício físico intenso e DAC permanece controversa, colocando-se a hipótese de associação tipo «curva em U». Neste contexto, a deteção subclínica de DAC em atletas veteranos pode ser justificada, estando propostas algumas metodologias. No entanto, a metodologia para a avaliação pré-competitiva dos atletas veteranos não é consensual e diversos marcadores de risco, adicionais aos fatores de risco CV clínicos tradicionais, poderão melhorar a estratificação de risco nesta população. Neste artigo revêm-se os dados publicados sobre DAC em atletas, com relevância para a relação entre a dose de exercício e DAC, bem como as implicações para a avaliação pré-competitiva de atletas veteranos.
Regular physical activity and exercise training have various health benefits, and are recommended for primary and secondary cardiovascular (CV) prevention.1,2 The benefits of exercise are mediated by multiple mechanisms, with favorable impact both in the general population and in patients with established CV disease in the context of cardiac rehabilitation. Among these effects are the prevention and control of various CV risk factors, including reduction in the incidence of obesity and diabetes and improved lipid and blood pressure profiles, as well as reduction of acute coronary events and increased survival.2
In response to the constant campaigns promoting the benefits of physical activity and exercise training, the number of people participating regularly in sports has grown in recent decades. Consequently, the spectrum of athletes has widened to include not only young adults, but also children and the elderly, with more individuals taking up regular exercise in middle age and continuing until late in life. Evidence of this tendency is the large number of veteran athletes involved in high dynamic component disciplines such as cycling, marathon, triathlon and Ironman races.3,4
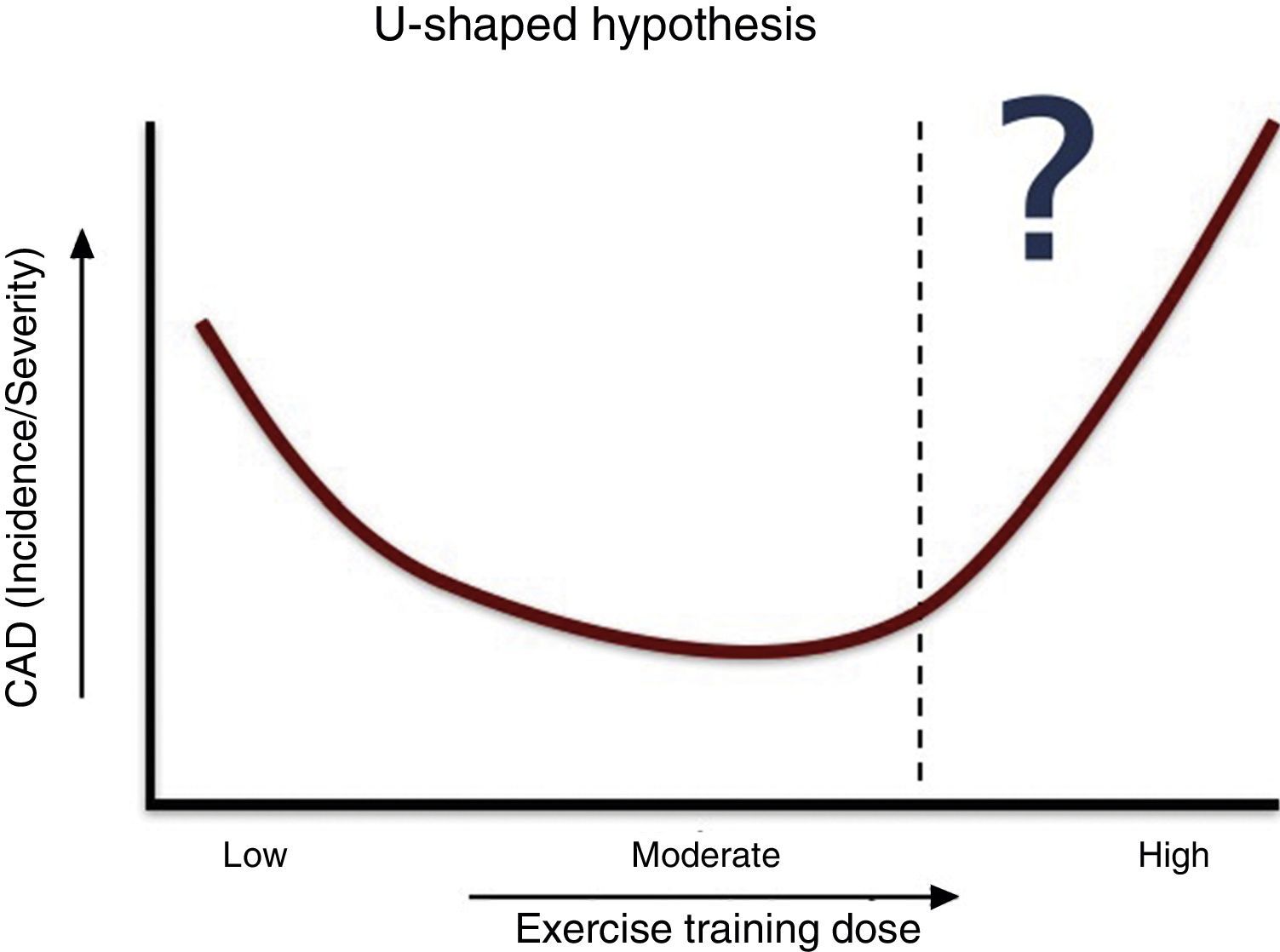
Although much is now known about exercise-induced physiological cardiac adaptations, the long-term effects of prolonged and excessive intense exercise training remain unclear. Recent evidence points to a potential U-shaped relationship between the dose of exercise and the occurrence of clinical CV events, which could be related to the presence and severity of coronary artery disease (CAD). This is an important issue, since CAD is responsible for the greatest proportion (approximately 80%) of sudden cardiac death (SCD) in veteran athletes, a less studied athletic population.
The recent development of new CV imaging tests, including non-enhanced cardiac computed tomography (CT) with calcium scoring (CS) and enhanced cardiac CT (coronary CT angiography [CCTA]), has enabled non-invasive detection and better characterization of the presence and severity of CAD.5 This could be a game-changer for risk stratification in veteran athletes, changing the paradigm from traditional stratification based on clinical CV risk factors and exercise electrocardiographic testing, which has well-known limitations.6
In the present paper we review the published data on CAD in athletes, focusing on the relationship between the dose of exercise and CAD, the potential mechanisms involved and the implications for pre-participation screening of veteran athletes, highlighting the role of CS and CCTA.
The paradox of sudden cardiac death in athletesDespite the proven benefits of regular physical exercise and although athletes are the paradigm of healthy individuals, this population is not risk-free and can suffer severe clinical conditions including SCD.5,7 Although SCD is uncommon in young athletes (incidence 2-5/100000 per year), it is a tragic event, with high visibility due to media attention. Most sports-related cardiac arrests occur in individuals not performing regular exercise, and in epidemiological terms, SCD during sports accounts for only a small proportion of cases in the general population.
Several studies have confirmed both the increased risk of exercise-associated myocardial infarction and SCD and the beneficial effect of regular exercise in risk reduction. Data from Italy revealed a 2.8-fold greater risk of SCD in young competitive athletes compared to non-athletes.8 However, it should be stressed that exercise is not the cause of death, but is a precipitating factor in susceptible individuals with previously undiagnosed cardiac disease. It should also be recognized that the overall beneficial effects of exercise in the population outweigh the increased risk.
In young athletes the most common causes of SCD are hereditary diseases, mainly cardiomyopathies and primary arrhythmic diseases, while in veteran athletes the great majority is caused by CAD.5,9–12 For the purpose of this paper, we define a veteran athlete as an individual more than 35 years old participating in sports at a competitive level or as a leisure activity. The majority of sports-related SCD occurs in older athletes, but as many of the deaths are unwitnessed, the magnitude of the problem is probably underestimated.12 Beyond the difference in the athletes’ age, other important epidemiological features of SCD in athletes are the higher frequency in males (9:1 to females) and occurrence during or immediately after exercise and mainly in high dynamic component sports.5
Identification of athletes with higher CV risk is a crucial goal of pre-participation screening.13,14 Although controversial, due to the long-standing disagreement between Europe and the US, the methodology recommended by the European Society of Cardiology (ESC) for screening of young athletes includes medical history (personal and family), physical examination, and 12-lead electrocardiogram (ECG).13 Central to the disagreement is the ECG, due to the high rate of false positive results. The main question is not whether the ECG should be included, but how it should be interpreted; the adoption of more restrictive criteria decreases the false-positive rate without reducing sensitivity and with a favorable impact on cost-effectiveness.15–19 Regarding the pre-participation screening of veteran athletes the controversy is greater, as will be discussed below.
Coronary artery disease in athletesSCD or acute myocardial infarction may be the first clinical presentation of CAD. The rupture of non-obstructive coronary plaques is the most common pathophysiological mechanism involved, which explains the previous absence of symptoms such as angina, usually present in individuals with obstructive CAD.9,20,21 Superficial plaque erosion and intraplaque hemorrhage are other mechanisms associated with coronary plaque instability, but ischemia due to an imbalance between oxygen supply and demand has also been described as one of the main causes of acute exercise-related cardiac arrest.20
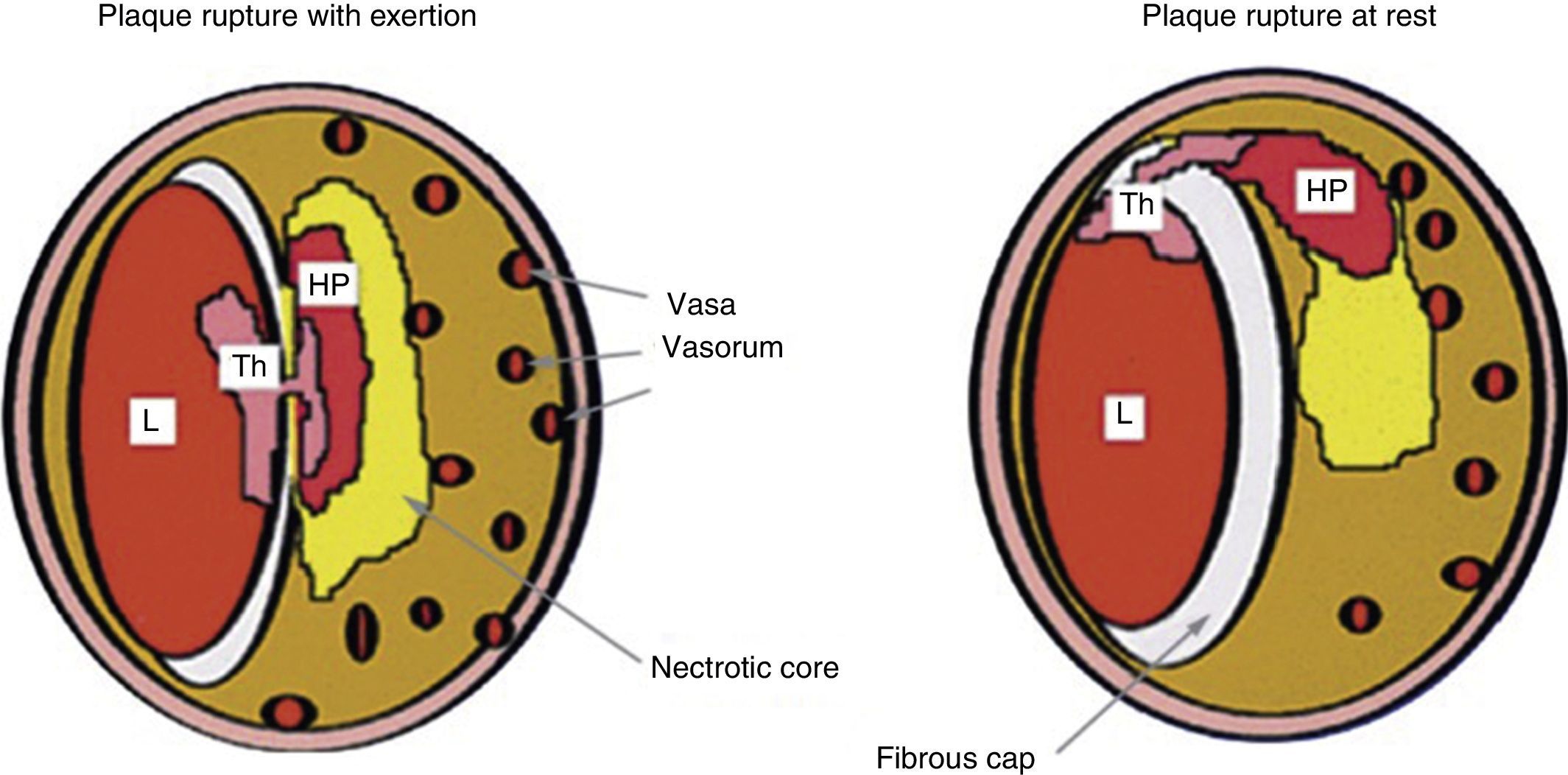
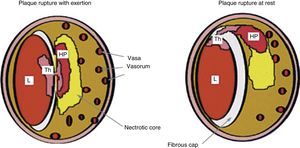
Plaque rupture during exertion typically occurs in the central part of a thin fibrous cap with numerous vasa vasorum, while plaque rupture at rest occurs more in the periphery, at the junction between the fibrous cap and the arterial wall (Figure 1).12,22
Comparison between coronary plaque rupture with exertion and at rest (reprinted from Burke et al.22). HP: hemorrhage into plaque; L: lumen; Th: thrombus.
Although the concept of advanced atherosclerosis in veteran athletes is somewhat counter-intuitive, various stress factors and pathophysiological mechanisms induced by chronic and extreme endurance exercise may play a critical role.
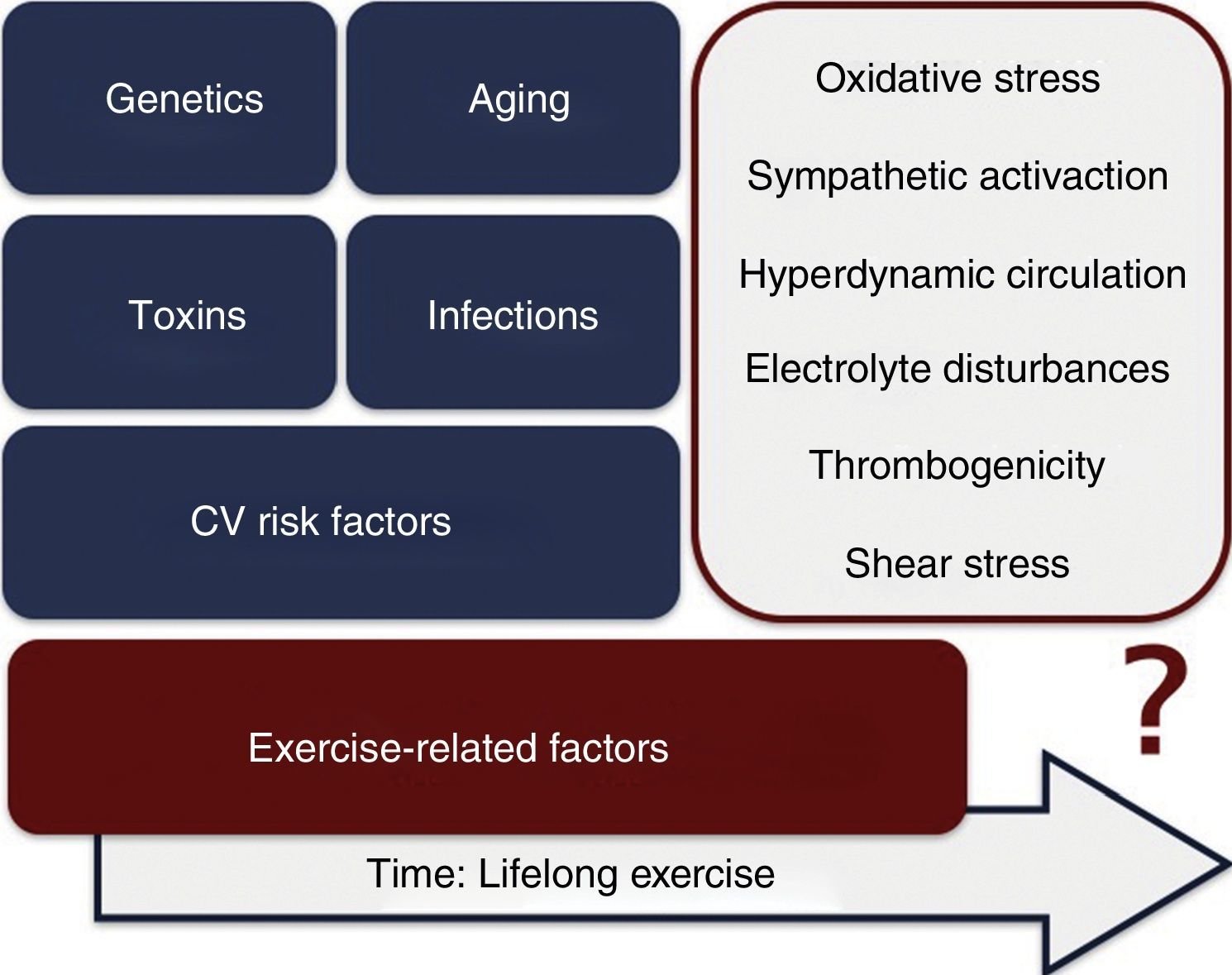
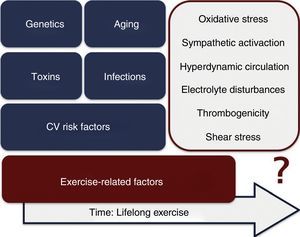
Among the potential mechanisms triggering exertion-related acute coronary syndromes are increased thrombogenicity, sympathetic activation, electrolyte imbalance, hyperdynamic circulation, shear stress and imbalance between the antioxidative and oxidative effects of exercise.12 An analysis performed in men with CAD exposed to physical exercise showed an improvement in antioxidant and vascular effects, a benefit which can be blunted with increased exercise intensity.23 Intense and prolonged exercise increases oxidative stress and release of inflammatory mediators such as oxygen free radicals and cytokines, a process documented in patients with CAD. Beyond the potential involvement of these exercise-related factors, it should be borne in mind that, as in the general population, the development of CAD in athletes is multifactorial, and can be affected by clinical CV risk factors, genetic predisposition, normal aging processes, infections and toxins (Figure 2).
Exercise training leads to the release of cardiac biomarkers, particularly troponin, an invaluable tool for the assessment of patients with myocardial infarction. In the context of exertion, this appears to be a benign process, but the underlying mechanisms are still poorly understood. Troponin elevation is likely to result from increased myocyte turnover, cellular release of proteolytic troponin degradation products, cellular wall permeability and formation and release of membranous blebs.24–26 Interestingly, the extent of troponin release is strongly related to intensity of exercise, and it is not clear if recurrent episodes would lead to long-term adverse cardiac effects.
Even with lower incidences, it is important to emphasize that besides the atherosclerotic process, there are other coronary abnormalities associated with SCD in athletes that should be considered and excluded, such as anomalous coronary artery origin, vasospasm, bridging, coronary dissection and vasculitis, which are beyond the scope of the present review.27,28
Relationship between amount of exercise and coronary artery diseaseThe relationship between amount of exercise and CAD is still not well established. In principle, as a drug becomes ineffective at a dose below that recommended, or toxic in the case of overdose, the same could happen with physical exercise. It is known that relatively modest doses of regular exercise are sufficient to induce benefits, but the upper limit above which the adverse effects outweigh the benefits has not been determined.29–32 There is emerging evidence that with increasing doses of exercise, the relative benefits decrease.30 Humans may not be genetically adapted for sustained intense exercise, and if so, it is worth considering how much exercise could actually be harmful and what the desired therapeutic window of exercise would be.
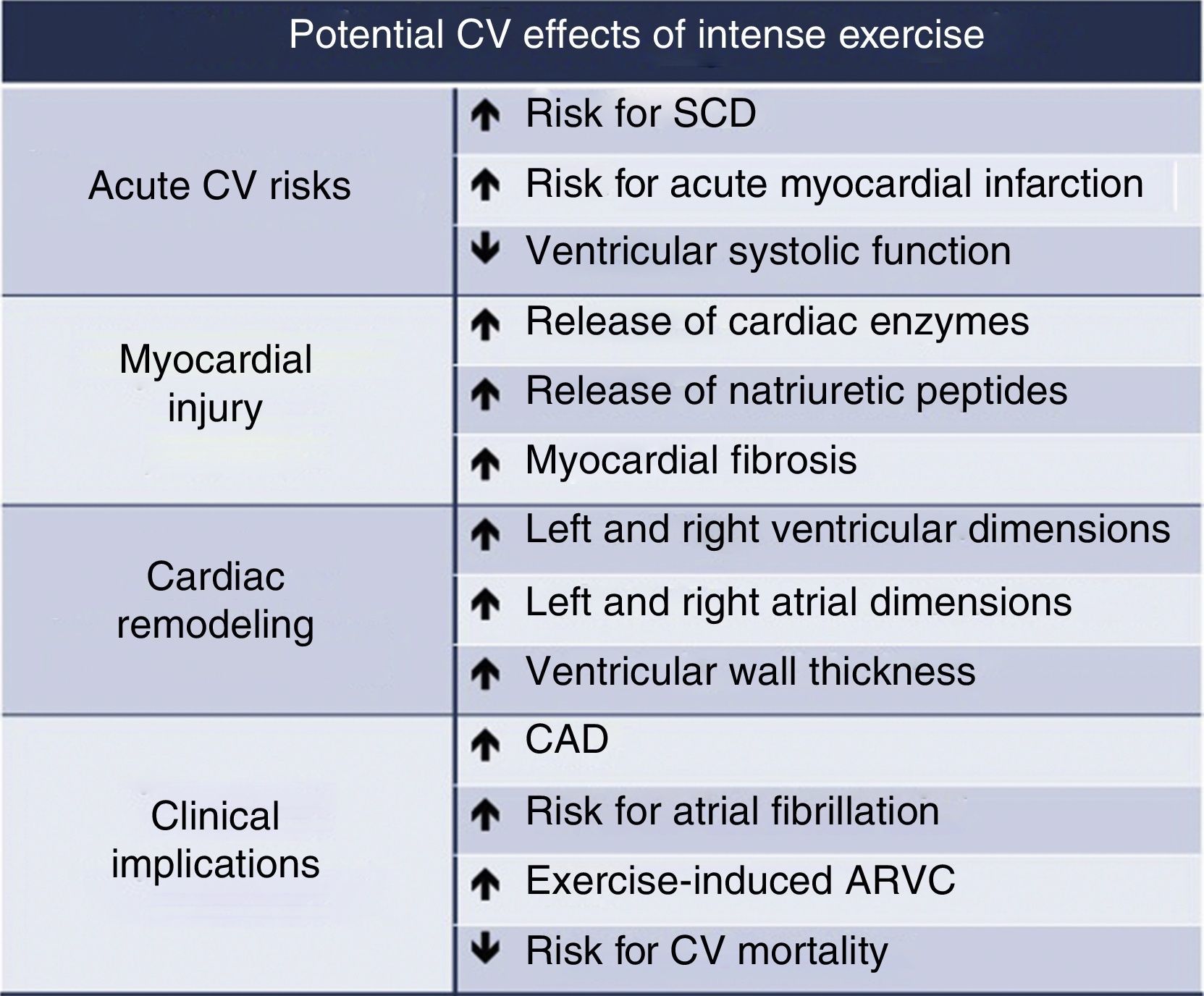
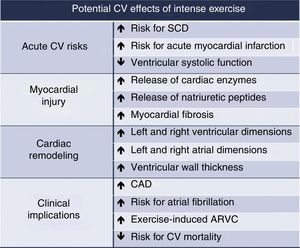
Extreme exercise leads to various cardiac changes (histological, structural and functional). These are mainly physiological adaptations, but maladaptation can also occur, increasing susceptibility to atrial and ventricular arrhythmias. Myocardial fibrosis, inflammation, marked ventricular remodeling and accumulation of coronary calcium are potentially related to extreme exercise (Figure 3).
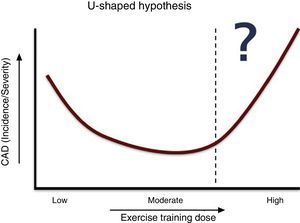
Some authors have argued that there exists a type of cardiotoxicity induced by extreme exercise, and the relationship between dose of exercise and incidence of clinical events has been described as a U-shaped curve.33,34 Moderate exercise appears to be better than none, but vigorous exercise may actually be harmful, at least for some individuals. From a public health perspective, we emphasize that although these findings raise some concerns about the benefits of high-end endurance sports, they do not undermine the substantial beneficial effects of regular exercise on all-cause mortality in the vast majority of older athletes.
Regarding mortality, this U-shaped relationship is clear for running distances, speeds and frequencies.35 In the Copenhagen City Heart Study,36 moderate joggers had lower mortality than sedentary nonjoggers and strenuous joggers. Although the evidence is weaker, the same relationship has been proposed for the presence and severity of CAD (Figure 4). In fact, the dose of exercise has a central role, as most cardiac arrests during marathons occur in the last quartile of races, although this could also be explained by cumulative electrolyte disturbances during the race.37
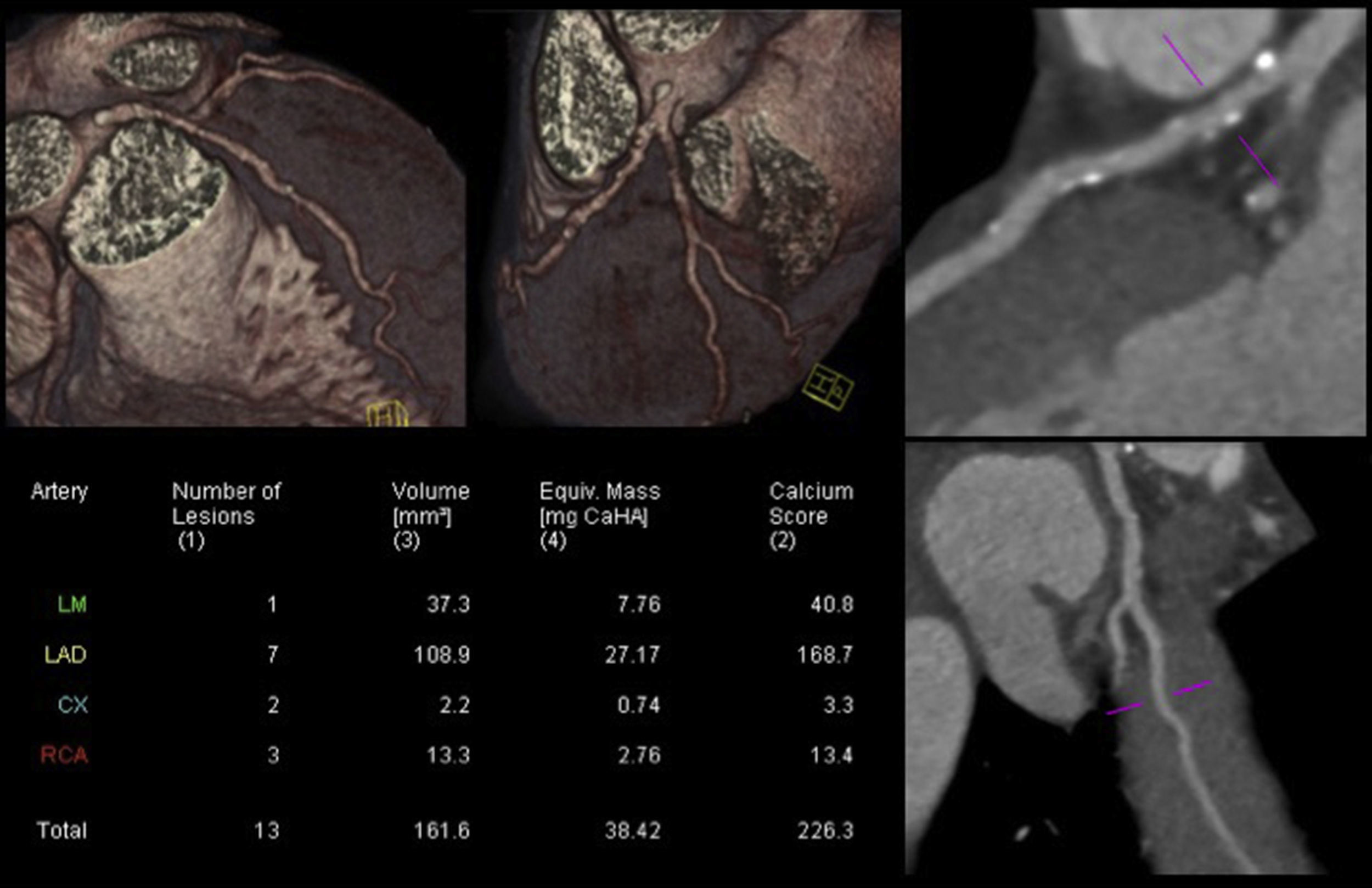
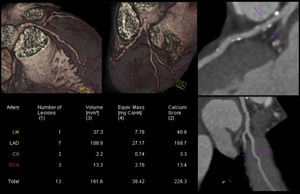
In daily clinical practice, it is not uncommon to identify athletes with a higher than expected atherosclerotic burden. Figure 5 illustrates a CCTA of an asymptomatic 47-year-old male competitive Ironman athlete, with a discrepancy between total CV risk based on SCORE (<1%) and extent of CAD.38
Coronary computed tomography angiography of a competitive Ironman veteran athlete with low cardiovascular risk based on SCORE (<1%), but with a higher than expected atherosclerotic burden (calcium score >percentile 90), with plaques in all the epicardial coronaries, including >5 segments with plaque (segment involvement score >5) and involvement of the left main and proximal left anterior descending arteries (adapted from Dores et al.38).
The potential association between intense exercise training and CAD does not appear to be an incidental finding. In recent years, several authors have described a higher than expected CAD incidence and severity in veteran athletes involved in endurance sports. Mohlenkamp et al.39 studied 108 veterans who ran at least five marathons over the previous three years, compared with a control group of non-athletes. CS was similar in both groups with adjustment for age, but significantly higher in the athletes after adjustment for Framingham risk score (mean CS: 36 vs. 12, p=0.02; CS ≥100: 36% vs. 22%, p=0.01; CS >percentile 75: 25% vs. 15%, p=0.01). During a mean follow-up of 21 months, athletes with CS ≥100 had a higher rate of CV events. Tsiflikas et al.40 studied male marathoners aged over 45 years and detected CAD in half of them, including 24% with plaques in the proximal coronary segments. Merghani et al.41 documented a U-shaped curve for the relationship between dose of exercise and CS in veteran athletes. A CS >percentile 70 was two or three times more frequent in athletes training >30 miles/week vs. <20 miles/week (39% vs. 13%; p=0.037). In the recent published MARC study,42 CCTA detected occult CAD in almost one in five asymptomatic sportsmen aged ≥45 years after a normal sports medical evaluation that included resting and exercise ECG. The number needed to treat in order to prevent one CV event compares favorably to that of other screening tests.
Despite these findings, several questions remain unanswered. These results imply that endurance athletes may not be protected from accumulation of coronary calcium, but it is important to recognize that the evidence does not show that endurance athletics has an adverse impact on either CS or CV events.12 It should also be emphasized that as well as being few in number, the published studies show inconsistencies: different inclusion criteria, regular exercise training begun at different ages, small samples, and different characterizations of exercise training.43 This issue requires a thorough analysis and more evidence, and is an emerging area of research in sports cardiology.
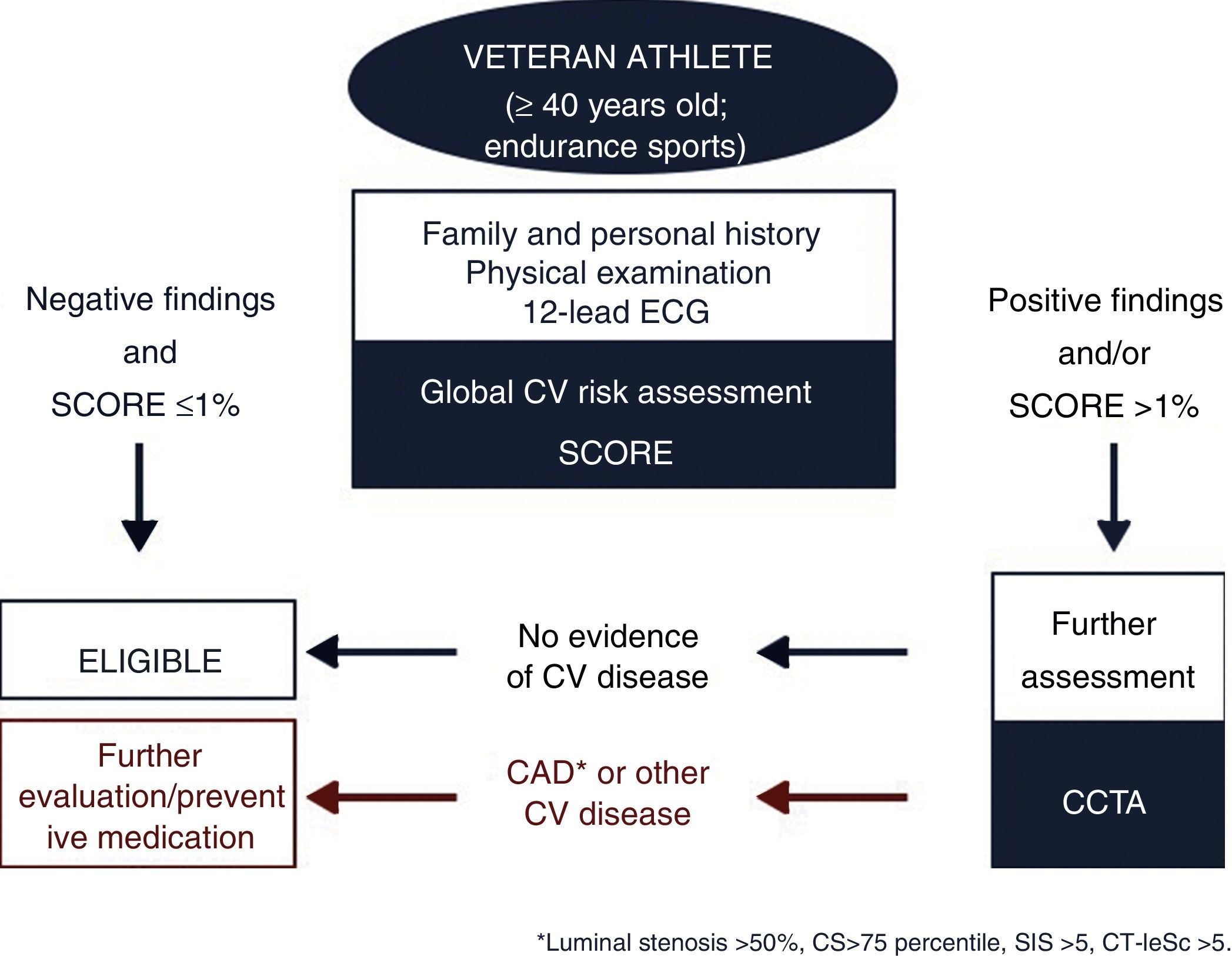
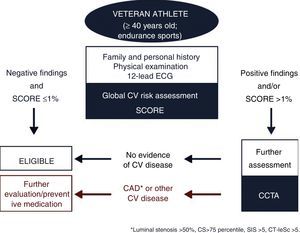
Cardiovascular risk stratification of veteran athletesThe epidemiological differences between young and veteran athletes justify the adoption of different pre-participation screening methodologies in the two groups. The large number of middle-aged individuals engaged in leisure-time sports makes the screening of this population an emerging task. Although the main cause of SCD in veteran athletes is coronary events, the focus of this screening should rule out subclinical CAD.12,44 Currently, a stepwise approach is suggested for the assessment of middle-aged/senior individuals involved in leisure or competitive sports:
- •
Step 1: Self-assessment using pre-specified questionnaires;
- •
Step 2: Assessment by a physician (personal and family history, physical examination, SCORE calculation and resting ECG);
- •
Step 3: Maximal exercise testing.
The identification and management of CAD in asymptomatic individuals (athletes or non-athletes) is a difficult task and there is still no agreement on the correct approach to adopt.45 Total risk estimation using multiple risk factors is recommended by the ESC for asymptomatic adults without evidence of CV disease (class I, level of evidence C).2 However, the predictive capacity of this conventional methodology based on clinical scores such as the Framingham risk score and SCORE is modest, failing to identify a significant proportion of individuals with established CAD. If these scores had been calculated on the day before an acute myocardial infarction, most patients would have had low-moderate risk, without indication for the implementation of preventive or therapeutic measures.46–48
Regarding the CV assessment of middle-aged/senior individuals engaged in leisure-time sports, the ESC recommends self-assessment of habitual physical activity level and risk factors, followed by SCORE calculation. Individuals with an increased risk for coronary events embarking on moderate/intense physical activity should undergo a maximal exercise test and possibly further cardiac investigation.49 Although this methodology may be valid in veteran athletes, it does not take into consideration specific characteristics such as dose of exercise, type of sport and length of exercise training. It seems obvious that more intensive investigation should be performed in athletes with moderate-high CV risk, particularly for those who are naïve or involved in high-level endurance sports. The main question is which further investigations should be performed.
Despite its recognized prognostic value, the utility of the ECG for screening asymptomatic subjects without known CAD is limited. Up to half of individuals with angiographically normal coronary arteries show changes on the ECG, one-third of those with CAD have normal baseline ECG, and the majority of coronary events occur in the absence of prior electrocardiographic abnormalities. In addition, all stress tests, by definition, depend on the presence of obstructive CAD and therefore they are not designed to detect nonobstructive CAD, which has been associated with worse CV outcome in several CCTA studies.50–54
Usually, athletes with high CV risk undergo an exercise ECG test, an exam of established prognostic value, widespread availability and low cost. Several studies have reported an increased relative risk of coronary death for asymptomatic subjects with a positive test. However, the accuracy of exercise testing for CAD detection in populations with low pretest probability, such as asymptomatic athletes involved in high-intensity sports, is limited.55–57 To overcome some of these limitations the measurement of biomarkers (e.g. high-sensitivity C-reactive protein and natriuretic peptides) has been proposed, but the gain in CAD detection and the practical applicability were low.58,59
Apart from the conventional scores based on clinical risk factors, it is known that some risk modifiers detected by emerging tests such as CS and carotid atherosclerotic plaque detection can improve the calculation of total CV risk.
The role of calcium score and cardiac computed tomography in screening veteran athletesDetermination of total atherosclerotic burden is an option for screening veteran athletes, helping to detect coronary calcifications, a recognized marker of subclinical atherosclerosis. CS is a non-invasive marker of CAD with proven prognostic impact, predicting CV events and death, independently of and incremental to conventional risk factors.60–63 CS is a risk modifier that can be considered in individuals with SCORE around 5%-10%. In the PESA study64 in individuals aged 40-54 years, 63% had subclinical atherosclerosis after assessment of multivascular territories, and CAD was detected in 18% of individuals, most of them with low SCORE. The landmark MESA study65 showed superior discrimination and reclassification of CV risk in intermediate-risk individuals using subclinical markers. CS had higher predictive power than other markers such as carotid intima-media thickness and ankle-brachial index, in agreement with the results of the Rotterdam study.66 Additionally, CS improves the adoption of preventive measures, leading to better control of several CV risk factors, as shown in the EISNER study.67,68
It is important to stress that not all coronary plaques are calcified, nor is CS an indicator of plaque instability. Moreover, although much less frequent than calcified or mixed plaques, non-calcified plaques are more prone to instability leading to acute coronary events. In this context, CCTA provides useful additional information, enabling better characterization of the coronary tree and plaques.26,69 Beyond obstructive CAD, the presence and quantity of non-obstructive plaques also has prognostic value, as shown in the CONFIRM registry70 and in other CCTA studies using atherosclerotic burden indices like the segment involvement score53 or the CT-adapted Leaman score (CT-LeSc).54 The comprehensive information provided by CCTA, including location, type and number of plaques, can be clustered in CCTA atherosclerotic burden scores like the CT-LeSc,71 which can help identify individuals with nonobstructive CAD at higher risk of CV events and therefore contribute to risk stratification.54
A recent study by Ermolao et al.57 in asymptomatic middle-aged athletes with ST-segment anomalies during maximal exercise test (diagnostic or equivocal) revealed CAD in only 32% of the subjects. In the MARC study,42 in 318 middle-aged sportsmen with low SCORE who underwent CCTA following normal pre-participation screening, 94% had low CV risk and 18.9% had CAD (CS ≥100 or ≥50% luminal stenosis), almost one in five individuals. In this setting, some authors have proposed the inclusion of CCTA in the screening of veteran endurance athletes with moderate-high CV risk. However, as Braber et al.42 showed, even veteran athletes with low CV risk could benefit from CCTA, increasing the controversy concerning the target population of this exam. Based on these data, mainly derived from studies performed in athletes aged >40 years involved in endurance sports and with a wide spectrum of CV risk (including low risk), a hypothetical flowchart for veteran athletes screening is proposed in Figure 6.
Another important feature of CCTA is the ability to detect other important coronary abnormalities in the screening of athletes, such as malignant variants of anomalous origin of the coronaries and coronary bridging, both described as possible causes of SCD in athletes.
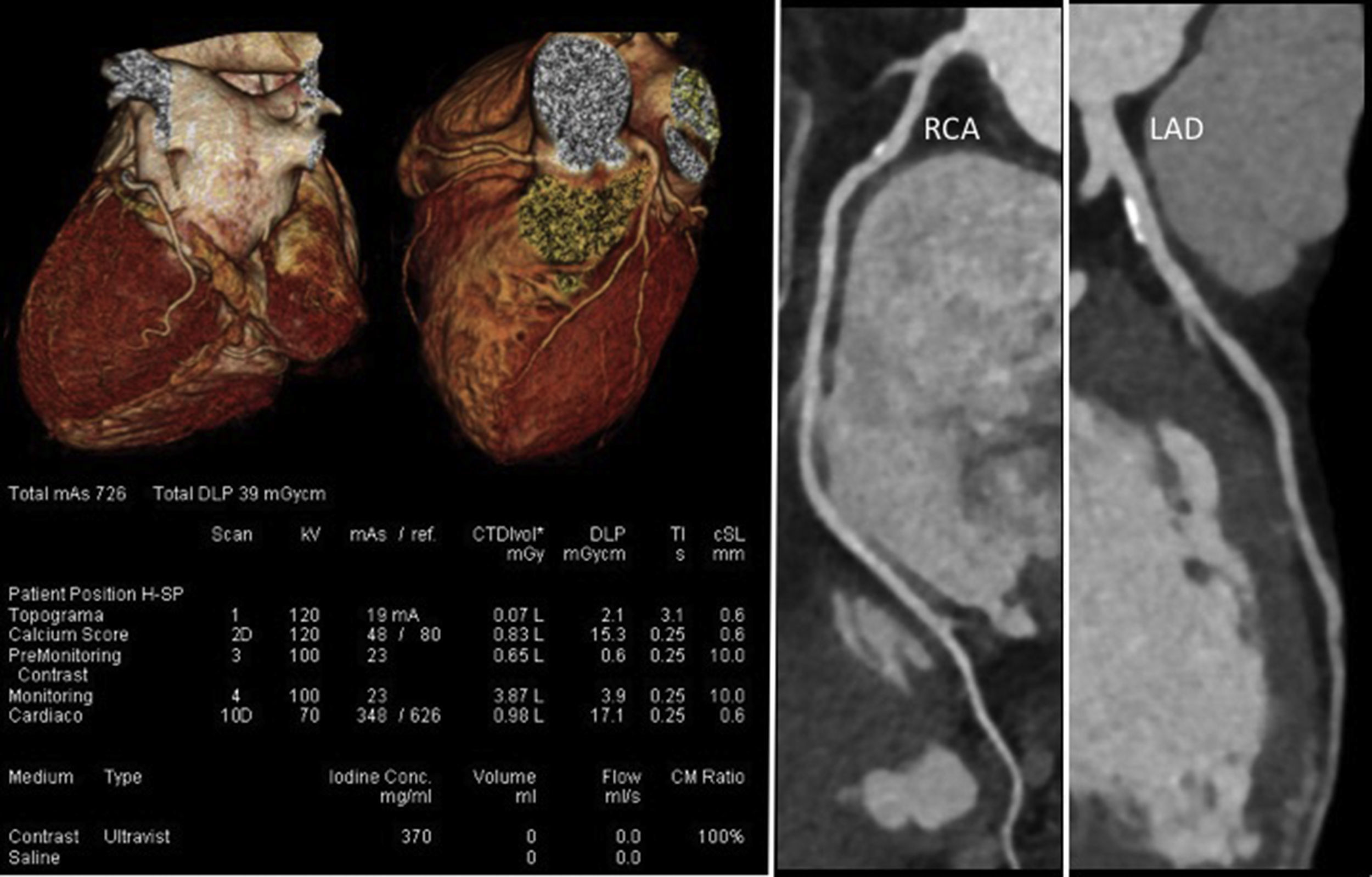
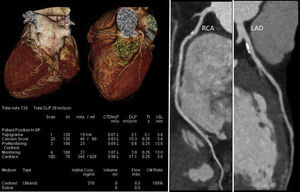
In addition, and also of considerable importance, recent technological developments in scanner technology (both hardware and software) have led to impressive reductions in radiation dose, the main limitation of CCTA.72,73Figure 7 presents an example of a CCTA performed with a new-generation scanner, showing high image quality with ultra-low radiation and contrast doses (0.5 mSv and 50 cc, respectively).
Coronary computed tomography angiography of a non-competitive athlete performed with a new-generation scanner (SOMATOM Force, Siemens Healthcare), using an ultra-low radiation dose of 0.5 mSv. Left: volume rendering technique images and study protocol; middle: nonobstructive mixed plaque in the proximal segment of the right coronary artery; right: nonobstructive calcified plaque in the proximal left anterior descending artery. LAD: left anterior descending artery; RCA: right coronary artery.
Finally, although we have reviewed the published evidence linking physical exercise and the presence and severity of CAD, several issues remain unanswered and warrant further research. It is the view of the authors that although CV risk stratification of veteran athletes is at present still based on traditional risk factors and rest ECG, cardiac CT may play a role in the future. To clarify this important issue, further research is needed focusing on three lines of investigation: first, to explore the possible U-shaped association between the dose of exercise and CAD; second, to establish the added value of CS and CCTA in screening of veteran athletes; and third, to demonstrate that the use of these newer CT-based imaging modalities can further improve risk stratification of this important subset of presumed healthy individuals, who may in fact be at risk of CV events.
ConclusionsThe benefits of exercise in the overall population are indisputable, but in athletes with CV disease exercise can also be associated with adverse clinical events, including SCD. In veterans, a growing group of athletes, CAD is the most common cause of SCD, and there appears to be an U-shaped relationship with the dose of exercise. Detection of subclinical CAD should be the main objective of veteran athlete screening, since the performance of classical CV risk stratification based on clinical factors appears to be suboptimal. Emerging data show an important role for CS and CCTA in this setting. Coupled with the impressive technical improvements in scanner technology in recent years, these have the potential to make cardiac CT a game-changer in the risk stratification of veteran athletes, with the ultimate goal of reducing the burden of CV events in this population, and should be the focus of further investigation in the near future.