We describe the case of a 59-year-old man who presented with chest pain and ST-segment elevation in the inferior leads, R>S in V1 and ST depression in the anterior leads due to proximal occlusion of the first obtuse marginal. Primary coronary angioplasty and stenting of this artery were performed. Twelve hours later the patient became hemodynamically unstable and severe mitral regurgitation due to rupture of one of the heads of the anterolateral papillary muscle was diagnosed. Emergency surgery was performed (papillary muscle head reimplantation, mitral annuloplasty with a rigid ring, tricuspid annuloplasty and coronary artery bypass grafting). On surgical inspection, it was observed that the detached muscle head had become trapped in the left ventricle by a secondary cord attached to the other head.
This case is unusual in presenting two uncommon features of ischemic papillary muscle: rupture of the anterolateral muscle in myocardial infarction involving the inferoposterior walls, and the fact that the ruptured muscle head did not prolapse because it had become trapped in the left ventricle by secondary cord attachment.
Apresentamos um caso de um homem, de 59 anos de idade, admitido no Serviço de Urgência por dor torácica e elevação ST nas derivações inferiores, r > s em V1 e depressão ST nas derivações precordiais, devido a oclusão da primeira obtusa marginal. Foi realizada angioplastia primária dessa lesão com implantação de stent revestido. Doze horas depois, o doente desenvolve instabilidade hemodinâmica, tendo sido diagnosticada uma insuficiência mitral grave por rutura de uma das cabeças do músculo papilar ântero-lateral. O doente foi submetido a cirurgia emergente (reimplantação do músculo papilar ântero-lateral, anuloplastia mitral com anel rígido, anuloplastia tricúspide e revascularização miocárdica). A inspeção cirúrgica revelou que a cabeça muscular rompida se mantinha presa ao ventrículo esquerdo por uma corda secundária que a ligava à outra cabeça do músculo papilar ântero-lateral.
Este caso tem a particularidade de apresentar 2 características incomuns da isquemia do músculo papilar: rutura do músculo ântero-lateral num enfarte póstero-inferior e o facto de a cabeça de músculo não prolapsar para a aurícula esquerda, por se encontrar presa ao ventrículo esquerdo por uma corda secundária.
Papillary muscle rupture is an infrequent but often catastrophic mechanical complication of acute myocardial infarction (MI) accounting for approximately 5% of early deaths.1 The condition may result in acute mitral regurgitation, acute pulmonary edema, and/or cardiogenic shock.2 Despite high operative mortality, surgery is indicated as survival of medically treated patients is very low.3
We report an uncommon presentation of an anterolateral papillary muscle rupture successfully repaired by surgical reimplantation of one of the papillary muscle heads.
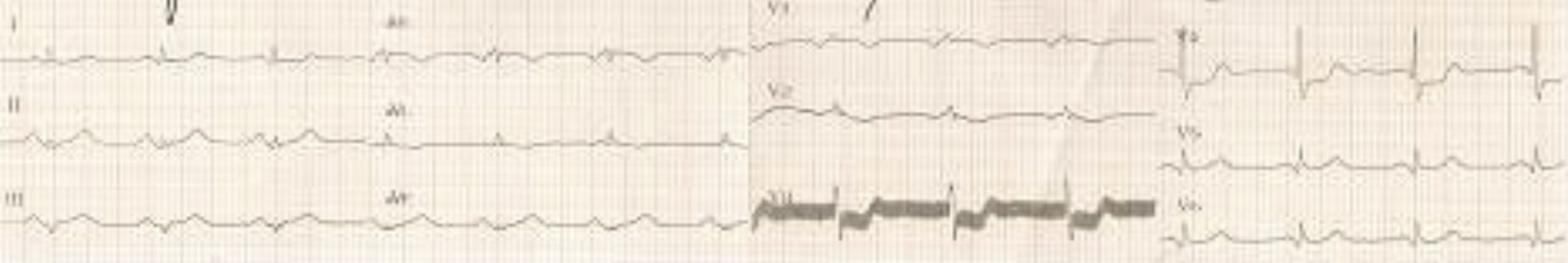
Case reportA 59-year-old man was admitted to the emergency room with acute chest pain. The 12-lead ECG (Figure 1) showed ST elevation in the inferior leads, R>S in V1 and ST depression in the anterior leads. The patient was hemodynamically stable and cardiac and pulmonary auscultations were normal.
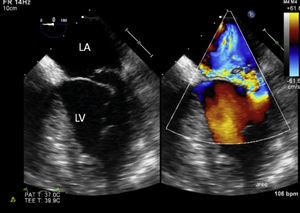
Coronary angiography showed obstruction of the proximal segment of the first obtuse marginal and significant stenosis (80%) of the proximal segment of the anterior descending artery. Primary coronary angioplasty of the first obtuse marginal and implantation of a drug-eluting stent were performed. Twelve hours later the patient suddenly became hypotensive and tachycardic. Physical examination revealed a new 3/6 holosystolic murmur at the apex and significant bilateral rales. Transthoracic echocardiography showed severe mitral regurgitation due to posterior mitral leaflet prolapse and an image of a mass in the left ventricle, which did not prolapse totally into the left atrium during systole, suggestive of an anterolateral papillary muscle head. Left ventricular size and function were relatively normal but the posterior and inferior walls were hypokinetic. Moderate tricuspid regurgitation was noticed and pulmonary artery systolic pressure was estimated at 60 mmHg.
The patient became oliguric, with deterioration of renal function, and so an intra-aortic balloon was placed and he was transferred to a cardiothoracic department for emergency surgery.
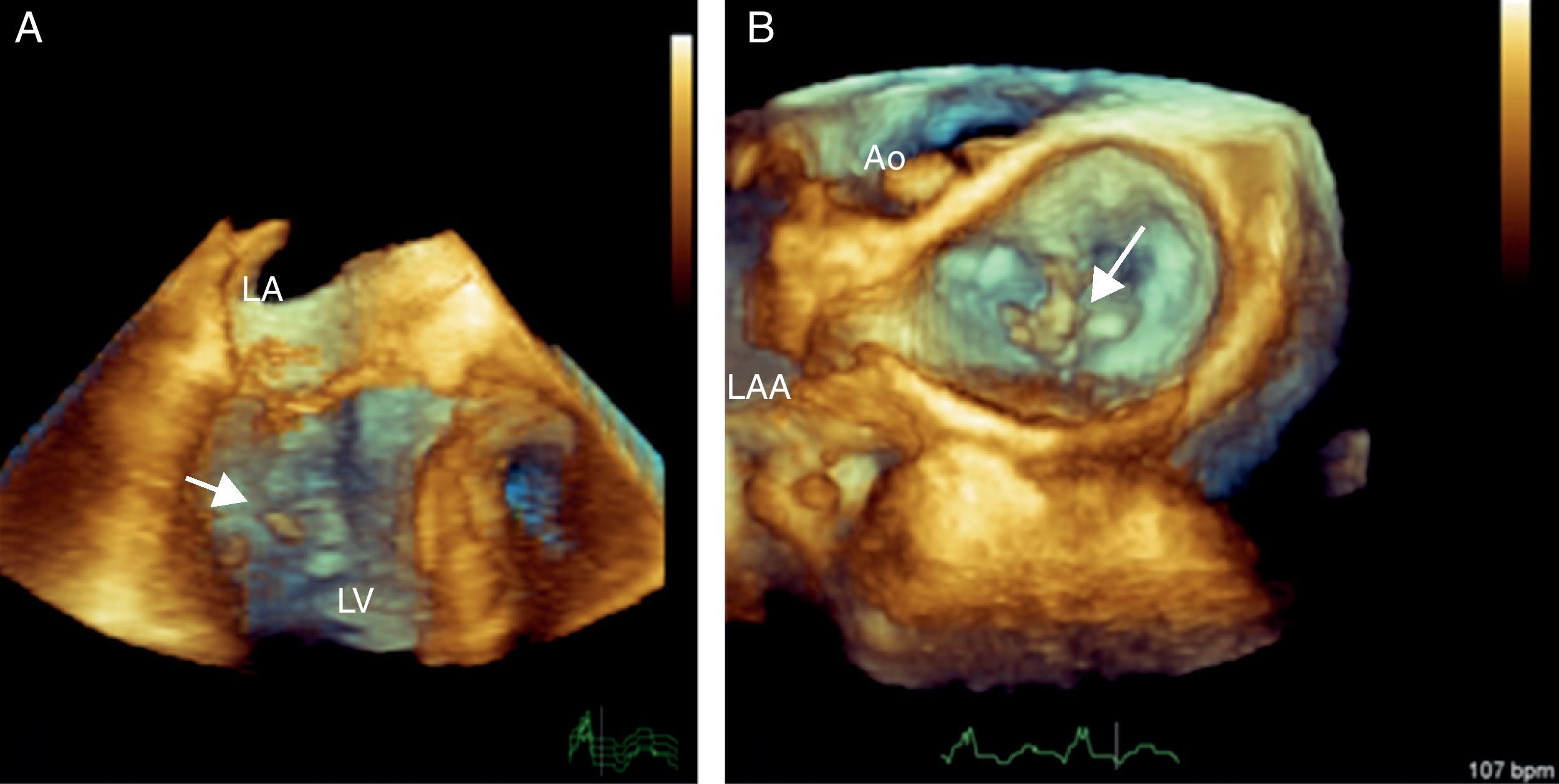
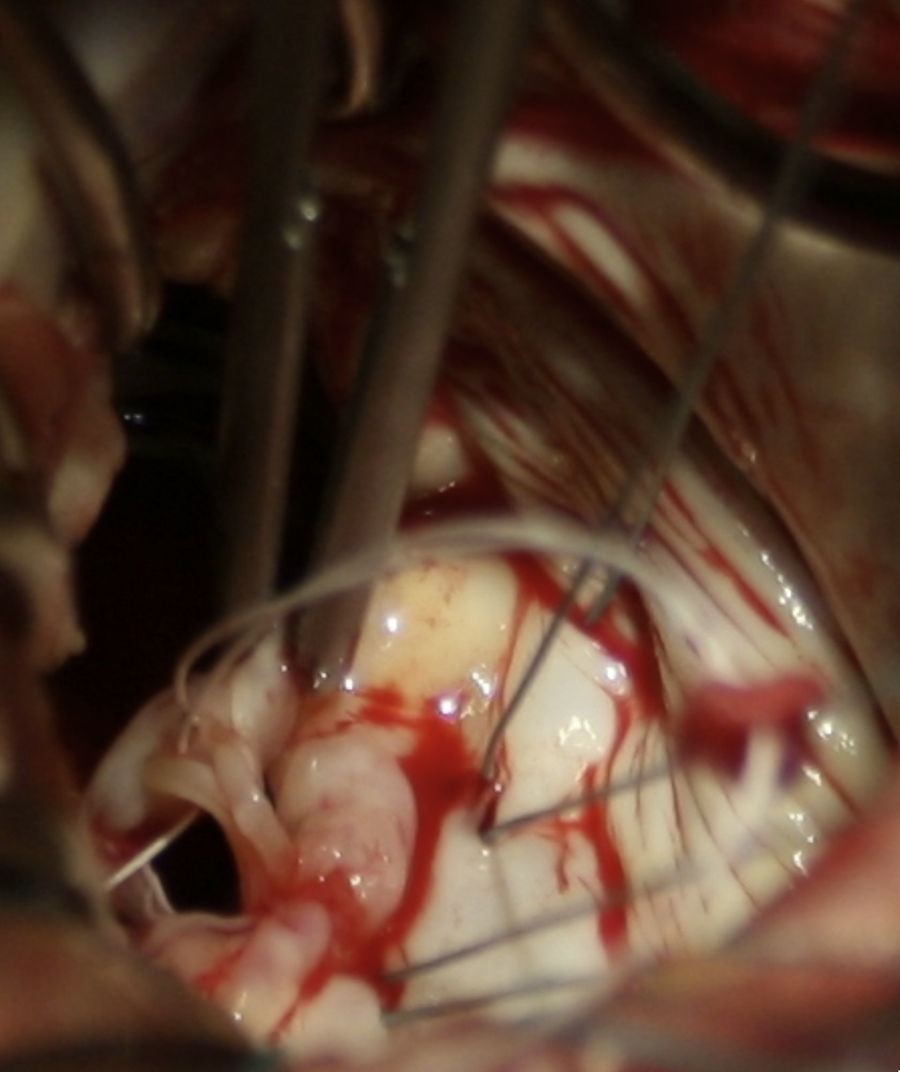
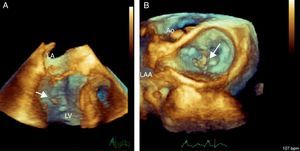
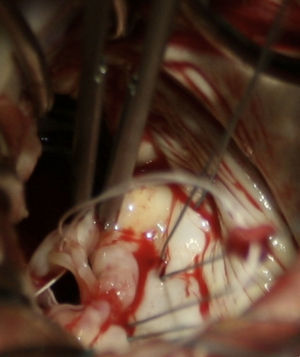
Intraoperative 2D/3D transesophageal echocardiography confirmed rupture of one of the heads of the anterolateral papillary muscle, leading to extensive prolapse of the P1 and P2 segments and causing severe mitral regurgitation (Figures 2 and 3A and B; videos 1, 2 and 3). On surgical inspection, it was observed that the detached muscle head (Figure 4) had become trapped in the left ventricle by a secondary cord attached to the other head. Papillary muscle head reimplantation, mitral annuloplasty with a rigid ring, tricuspid annuloplasty with a Sovering ring and double coronary artery bypass grafting (CABG) (left internal mammary artery to first obtuse marginal and right internal thoracic artery to anterior descending artery) were performed.
Three-dimensional transesophageal echocardiography. (A) Full volume cropped image showing the detached head of the anterior papillary muscle inside the LV (arrow) causing severe prolapse of the posterior leaflet; (B) 3D Zoom of the mitral valve showing prolapse of the P1 and P2 segments. LA: left atrium; LV: left ventricle; Ao: aortic valve; LAA: left atrial appendage.
The postoperative period was complicated by nosocomial pneumonia but the patient recovered fully and was discharged home on the 18th day. Transthoracic echocardiography performed 15 days after surgery showed preserved global left ventricular function and mild mitral regurgitation.
DiscussionThe posteromedial papillary muscle is supplied with blood from the posterior descending artery, while the anterolateral papillary muscle has a dual blood supply, from the left anterior descending and left circumflex arteries.4–6 This difference in blood supply explains why rupture of the posteromedial papillary muscle is 6–12 times more common. On the other hand, rupture of the anterolateral papillary muscle is usually associated with anterolateral MI, rarely occurring in the context of inferior MI, as happened in the case presented.7
Transthoracic echocardiography is useful in the diagnosis of papillary muscle rupture, with a sensitivity of 65–85%.8 A flail segment of the mitral valve and a severed papillary muscle or chorda can frequently be seen moving freely within the left ventricular cavity. However, in some cases, transthoracic echocardiography is not informative and transesophageal echocardiography is required to establish the diagnosis; this is most likely to occur when the ruptured head does not prolapse into the left atrium, as was observed in our patient, a feature reported in up to 35% of cases.9
Emergency surgical intervention remains the treatment of choice for papillary muscle rupture. Surgery involves significant operative mortality (18%), but there are recent trends for lower operative risk, particularly with associated CABG (8.7%).10 Long-term outcome after surgery is the same as that of similar MI without papillary muscle rupture.10 These encouraging observations emphasize the importance of prompt diagnosis and an aggressive therapeutic approach for patients suffering papillary muscle rupture after MI.
This case is unusual in presenting two uncommon features of ischemic papillary muscle: rupture of the anterolateral muscle in MI involving the inferoposterior walls, and the fact that the ruptured muscle head did not prolapse because it had become trapped in the left ventricle by a cord attachment.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.