Reflex vasovagal syncope often affects young populations and is associated with a benign prognosis in terms of mortality. However, a minority of patients have recurrent episodes, with a considerable impact on their quality of life.
Pacemaker therapy has been an option in these patients since the 1990s if a conservative strategy fails. Initially, non-randomized and open-label randomized trials showed promising results, but these studies were associated with a significant placebo effect. Recently, an approach based on the use of implantable loop recorders has shown that some patients with reflex vasovagal syncope could benefit from implantation with dual-chamber pacemakers, particularly patients aged >40 years, with recurrent syncopal episodes resulting in frequent injuries, in whom a long asystole (≥3 s asystole with syncope or ≥6 s asystole without syncope) has been documented with an implantable loop recorder.
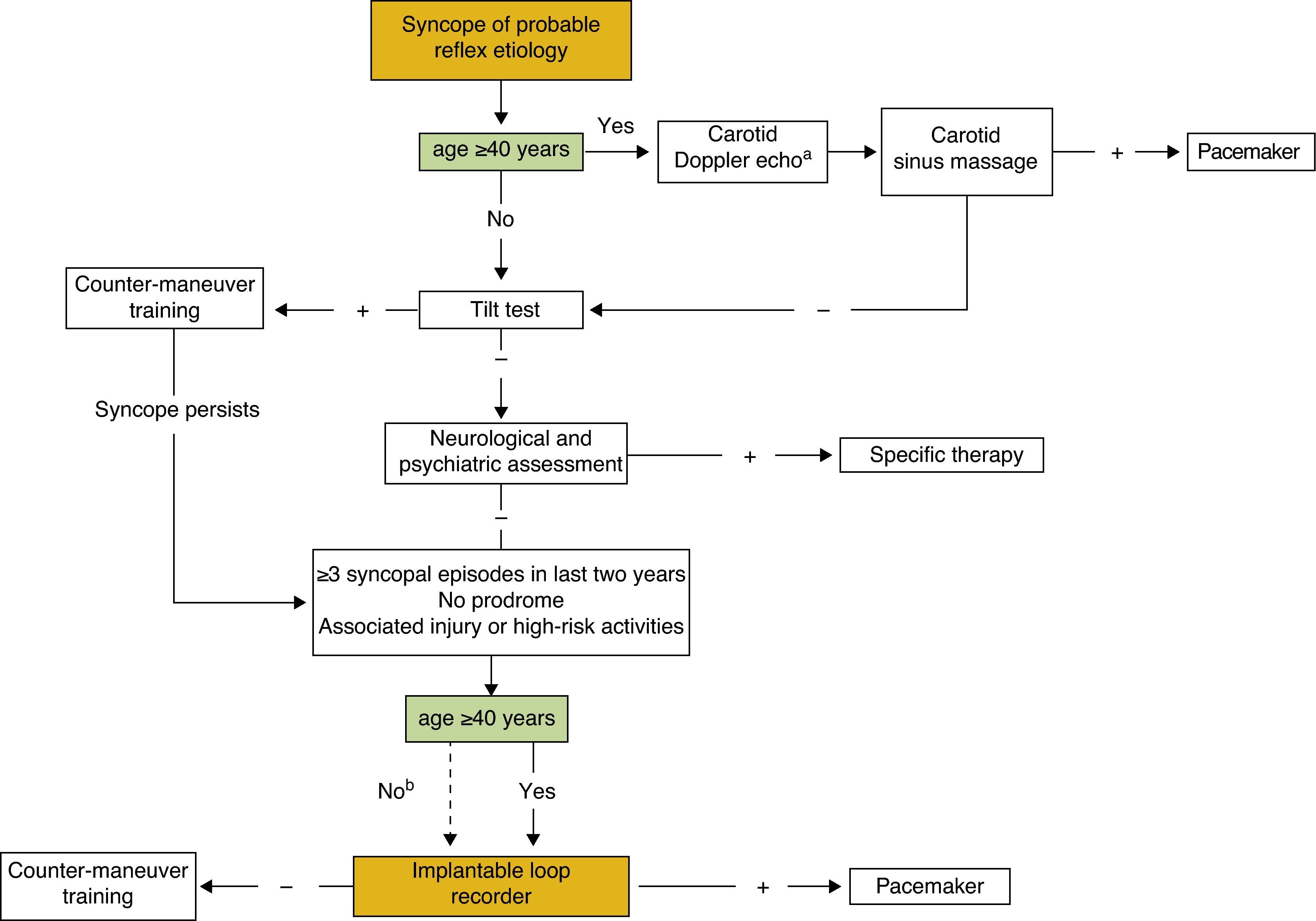
The authors present a literature review on the role of cardiac pacing in reflex vasovagal syncope and propose a diagnostic and therapeutic decision flowchart for patients with syncope of probable reflex etiology.
A síncope reflexa vasovagal afeta frequentemente uma população jovem estando associada a um prognóstico benigno em termos de mortalidade. No entanto, uma minoria de doentes apresenta episódios recorrentes com grande repercussão na sua qualidade de vida.
Desde meados dos anos 90 que a terapêutica com pacemaker tem sido proposta neste grupo de doentes, em caso de insucesso da estratégia conservadora. Inicialmente, os estudos não aleatorizados e aleatorizados e os estudos aleatorizados abertos mostraram resultados promissores, associados, no entanto, a um considerável efeito placebo. Recentemente, uma abordagem baseada na utilização do detetor de eventos implantável revelou que alguns doentes com síncope reflexa vasovagal podem beneficiar da implantação de pacemaker de dupla câmara, nomeadamente doentes com mais de 40 anos, com episódios recorrentes de síncope, com consequências graves para os doentes, e com documentação de uma longa assistolia (≥3 s de assistolia com síncope ou ≥6 s de assistolia sem síncope) no detetor de eventos implantável.
Os autores efetuaram uma revisão da literatura relativamente ao papel do pacing cardíaco na síncope reflexa vasovagal e propõem um algoritmo de decisão diagnóstica e terapêutica para os pacientes com síncope de provável etiologia reflexa.
Syncope is defined as a transient loss of consciousness due to transient global cerebral hypoperfusion characterized by rapid onset, short duration, and spontaneous complete recovery.1 Its incidence, based on the Framingham study, is estimated at 6.2 per 1000 person-years,2 while the prevalence of at least one lifetime episode may reach 50%.3,4
The most common form is reflex vasovagal syncope, which more often affects young populations and is associated with a benign prognosis, especially in terms of mortality.2 Therapeutic strategies reflect this benignity, consisting mainly of lifestyle modification and maneuvers to abort syncopal episodes. Randomized trials have not provided solid evidence of the value of other interventions, such as tilt training5–9 and pharmacological therapy.1 Despite these measures, a minority of patients present recurrent syncopal episodes, with an impact on their quality of life that is comparable to that of other chronic diseases, such as chronic renal disease or recurrent depressive disorder.10–12
Pacemaker therapy has been proposed for patients with recurrent vasovagal syncope who do not respond to non-invasive measures. According to the European guidelines,13 cardiac pacing should be considered in patients with reflex vasovagal syncope aged ≥40 years with recurrent, unpredictable syncope after a correlation has been established between symptoms and a sinus pause and/or atrioventricular block (class IIa recommendation, level of evidence B), and may be considered in patients with tilt-induced cardioinhibitory response with recurrent syncope and age >40 years after alternative therapy has failed (class IIb recommendation, level of evidence B). Pacemaker therapy in patients with reflex vasovagal syncope is still the subject of controversy.
The authors present a literature review on the role of cardiac pacing in reflex vasovagal syncope and propose a decision flowchart for patients with syncope of probable reflex etiology.
Rationale for pacing in reflex vasovagal syncopeReflex syncope is caused by an inadequate cardiovascular response that results in hypotension and/or bradycardia. It is commonly classified according to the predominant type of response during tilt testing: type 1, mixed (with hypotension and bradycardia); type 2A, cardioinhibitory, predominantly bradycardia; type 2B, cardioinhibitory with asystole; and type 3, vasopressor (predominantly hypotension).1 The aim of pacing therapy is to prevent significant bradycardia or asystole and to raise heart rate in order to counteract hypotension.
Initial evidence in favor of pacingNon-randomized trialsThe use of pacing in certain patients with reflex syncope has been accepted since the 1990s, although there is considerable disagreement concerning the results. This disagreement is reflected in a review by Wijesekera and Kurbaan,14 which showed that temporary pacing was beneficial during tilt testing in some trials, while in others pacing did not consistently prevent syncopal episodes.10 Later non-randomized trials15–17 in patients with cardioinhibitory syncope during tilt testing showed that implantation of a dual-chamber pacemaker reduced or even eliminated syncopal episodes in most patients.
Open-label randomized trialsOf the open-label randomized trials on this subject, three – VPS I,18 VASIS19 and SYDIT20 – are particularly important as they provided evidence in favor of pacing for vasovagal syncope.
The VPS I18 trial included 54 patients with a history of at least six episodes of syncope who presented bradycardia with syncope or pre-syncope on tilt testing. They were randomized to two groups, one with and the other without a dual-chamber pacemaker with a rate-drop response algorithm. The study was terminated early after an interim analysis showed a marked reduction in syncope in the pacemaker group (22% vs. 70%, p<0.001).
The VASIS study,19 published in 2000, included 42 patients with ≥3 syncopal episodes in the previous two years and type 2A or 2B cardioinhibitory response to tilt testing (86% of patients presented a systolic pause of >3 s, with a mean ventricular pause of 13.9±10.2 s). The participants were randomized to receive a dual-chamber pacemaker with rate hysteresis or to control. There was a significant reduction in recurrent syncope in the pacemaker group (5% vs. 61%, p<0.001) compared to the control group.
The randomized SYDIT trial,20 published in 2001, compared dual-chamber pacing (with rate-drop response function) and beta-blocker therapy. The 93 patients were aged >35 years, had had ≥3 syncopal spells in the preceding two years and presented syncope with bradycardia on tilt testing. The trial was terminated early when an interim analysis showed a marked reduction in recurrent syncope in the pacemaker group (4.3% vs. 25.5%, p=0.004).
Evidence against the effectiveness of pacing – a placebo effect?Double-blind randomized trialsThese open-label randomized trials had an important limitation, in that the benefit reported may have been due to a placebo effect associated with the surgical procedure.21–23
Two double-blind randomized trials have set out to overcome this limitation: VPS II and SYNPACE.
In VPS II,24 100 patients with at least six episodes of syncope ever, or at least three episodes in the two years prior to enrollment, and positive tilt test, were implanted with a dual-chamber pacemaker with rate drop response pacing and then randomized to two groups, one with active pacing and the other with sensing without pacing. At six months, there was no statistically significant difference between the groups (p=0.14) in recurrence of syncope, which was recorded in 22 of the 52 patients with inactive pacing (42%) and in 16 of the 48 patients with active pacing (33%). It is worth noting that in the first VPS trial,18 around 80% of the no-pacemaker group had recurrent syncope at six months, while only 42% of the sensing-only group in VPS II presented recurrence at six months.24
Eligibility for the SYNPACE trial25 was at least six syncopal events in the patient's lifetime and positive tilt test. The trial was terminated early following the publication of the VPS II results and the first interim analysis, at which point 29 patients had been randomized for pacemaker implantation, some with active and others with inactive pacing. A high proportion (50%) of patients had recurrent syncope despite active pacing, a similar percentage to that seen for inactive pacing (38%).
These two double-blind randomized trials undermined belief in the value of pacing in reflex vasovagal syncope, suggesting that the benefit seen in previous studies was due to a placebo effect. The ineffectiveness of active pacing was not surprising and is probably explained by the inability of cardiac electrical stimulation to counteract the vasopressor component of the vasovagal reflex that is present in most syncopal episodes and usually precedes the cardioinhibitory response and bradycardia.25
The role of implantable loop recordersIn view of these conflicting results, the possibility was raised that the explanation lay in patient selection. An analysis of the SYNPACE trial showed that the mean time to first syncopal relapse tended to be longer in patients with active pacing and asystole on tilt testing,25 which suggests that pacemaker therapy in patients selected on the basis of the presence of asystole on tilt testing could be beneficial.
However, doubts have also been expressed as to whether tilt testing is in fact the best method of selecting patients for pacemaker implantation, since patients with vasovagal syncope present different rhythm disturbances during spontaneous syncope from those seen during syncope induced by tilt testing.26,27
Implantable loop recorders (ILRs) can show whether spontaneous syncope correlates with the electrocardiogram (ECG). In patients with unexplained syncope, ILRs have shown a correlation in 35% of cases, of which 56% presented asystole (or significant bradycardia in a few cases) during the event.28–36 In a recent study by Furukawa et al.,37 the rate of diagnosis reached 80% after four years of follow-up.
The ISSUE 2 trial38 was a prospective multicenter study in which ILRs were implanted in 392 patients at least 30 years of age who had suffered three or more syncopal episodes in the previous two years. After up to two years of follow-up, the 103 patients who presented recurrent syncope were randomized, with 53 receiving specific therapy (47 a pacemaker, four tachycardia ablation, one an implantable defibrillator, and one anti-arrhythmic medication) and the remaining 50 (49%) not receiving any specific therapy. Those who received specific therapy had a significant reduction in syncope recurrence at one year (10% vs. 41%, p=0.002) compared to those without specific therapy. Patients with recurrent vasovagal syncope and asystole documented by the ILR who received a pacemaker had a more than 80% relative risk reduction for syncope recurrence.38 However, the ISSUE 2 trial was not double-blinded, and therefore the question of a possible placebo effect remains.
ISSUE-3: validation of pacing in reflex vasovagal syncopeThe ISSUE-3 trial39 was a double-blind, randomized multicenter study of patients aged ≥40 years who had experienced ≥3 syncopal episodes in the previous two years. ILRs were implanted in 511 patients, 89 of whom had documented syncope with ≥3 s asystole or ≥6 s asystole without syncope but with asymptomatic or presyncopal episodes. Of these 89 patients, 77 received a dual-chamber pacemaker with rate drop response and were randomized to pacing or sensing without pacing. These 77 patients had a mean age of 63±13 years, several syncopal episodes (a median of four events in the last two years), older age at first syncope, and two-thirds had been hospitalized for syncope; they had suffered various syncope-related injuries (43% minor and 8% major injuries), which may have been due to atypical presentation (56% of cases), and around 80% had presented syncope with documented asystole of ≥3 s (mean pause 11±4 s).
In addition, 33 (87%) of the pacing group and 32 (82%) of the non-pacing group underwent tilt testing, which was positive in only 42% of the pacing group and in 72% of the non-pacing group. By way of comparison, 79% of the pacing group presented syncope, compared to 82% of the non-pacing group, which demonstrates the low correlation between tilt test results and occurrence of spontaneous syncope. During two-year follow-up, syncope recurrence was observed in 19 patients in the non-pacing group and in eight in the pacing group; the recurrence rate was thus significantly lower in the pacing group (25% vs. 57%, p=0.039).39
The ISSUE 2 and ISSUE-3 trials showed that pacemaker therapy can be beneficial when there is documented asystole in spontaneous syncope. However, even in such cases the hypotensive component is also important, as demonstrated by the 25% of patients with active pacing who suffered recurrent syncope despite pacemaker therapy.39
Complications associated with pacemaker therapyPacemaker implantation is not without risk of complications. In a recent prospective study by Udo et al.,40 the short- and long-term complication rates after first pacemaker implantation for bradycardia were 12.4% and 9.2%, respectively.
The adverse event rate in the VPS I trial18 was 26% (five patients) in the pacemaker group, including one lead dislodgement, while in VPS II24 the rate of pacemaker-related complications was 19%, including one patient with pericardial tamponade, one with infection requiring reimplantation of the generator, one with vein thrombosis and seven with lead dislodgement or repositioning. In the ISSUE-3 trial,39 five patients (6.5%) had procedure-related complications: ventricular lead dislodgment in two, atrial lead dislodgment in two, and subclavian vein thrombosis in one.
The long- and short-term complication rates associated with pacemaker implantation are not negligible, and should always be borne in mind when deciding on the treatment of patients with a condition that is benign in terms of mortality.
Proposed decision flowchartThe authors recently proposed a diagnostic flowchart for patients with syncope of probable reflex etiology.41
We now propose a revised version of the flowchart, designed to stratify patients for appropriate treatment, not merely to establish an etiological diagnosis (Figure 1).
Decision flowchart for syncope of probable reflex etiology. aOnly in patients with stroke/transient ischemic attack in the previous three months or carotid bruit.1bHigh-risk professions or activities. Echo: echocardiography.
Following initial assessment including clinical history, physical examination and ECG, and having excluded structural heart disease, investigation of patients with probable reflex syncope should be primarily guided by the patient's age.
In those aged ≥40 years, carotid sinus massage should be performed after carotid Doppler to exclude atherosclerotic plaques if the patient has stroke/transient ischemic attack in the previous three months or carotid bruit.1 If carotid sinus massage is positive, i.e. syncope is induced with documented asystole of >3 s, a pacemaker should be implanted.1
If carotid sinus massage is negative, a reflex vasovagal etiology can be confirmed by tilt testing, but only if the symptoms correlate with those of spontaneous syncope. Tilt testing can also indicate whether the cardioinhibitory or the vasopressor component is predominant, although it is debatable to what extent this correlates with spontaneous syncope.
Patients with a positive tilt test (reproducing symptoms together with hypotension, bradycardia or both) are taught maneuvers to abort vasovagal syncope. Those who do not suffer recurrence after such training require no further investigation or treatment. Those with a negative tilt test should be referred for neurological or psychiatric assessment and appropriate treatment instituted if such a cause is confirmed.
Otherwise, patients with a negative tilt test and those who continue to suffer recurrent syncope (≥3 episodes in the last two years) despite training, with no or very short prodromes and with frequent injuries or in high-risk professions, should receive an ILR.
Patients aged <40 years should undergo tilt testing, notwithstanding the limitations of this exam. Those with a positive test should be trained in counter-maneuvers to abort syncopal episodes, and if they do not suffer recurrence, no further investigation is needed. If the test is negative, patients should be referred for neurological and psychiatric assessment, and if these etiologies are excluded, they should be trained in counter-maneuvers.
In patients with high-risk professions or activities, multiple injuries, or recurrent syncopal episodes that significantly impact quality of life, an ILR may be considered, but this should be used sparingly in those aged <40 years.
Patients in whom the ILR documents syncope with ≥3 s asystole or ≥6 s asystole without syncope should receive a pacemaker; otherwise, they should continue counter-maneuver training and be kept under clinical surveillance, since in most the vasopressor component is likely to predominate.
Pacemaker implantation is not without risk of complications, and the risk-benefit ratio should thus be considered on an individual patient basis, particularly for younger patients, given their greater cumulative risk.
Outstanding issuesThere are still several outstanding issues on this subject.
Although the usefulness of pacemaker therapy is increasingly called into question, there has still been no double-blind randomized trial in which patients with type 2B syncope (with asystole or significant bradycardia) on tilt testing are selected for active or inactive pacing.
It is not clear whether a rate-drop response algorithm is ideal. It is possible that the use of different sensing modalities, such as those based on cardiac contractility or respiratory changes, might yield better results in preventing syncopal relapse.25
There is also considerable uncertainty regarding which patient groups will benefit most from pacemaker therapy. The ISSUE-3 trial39 did not have sufficient statistical power for subgroup analysis, and so this question remains open.
It is not known whether asymptomatic patients with documented asystole would benefit from pacemaker implantation. In the ISSUE-3 trial,39 of the 38 patients with active pacing, only 21% had pre-syncope or were asymptomatic (non-syncopal pause on the ILR), which is insufficient to determine the benefit of pacing in this patient group.
In the ISSUE-3 trial, patients’ mean age was 63±13 years and 56% had atypical presentation. This suggests that the etiology of their syncope may not have been vasovagal reflex but a different pathophysiological mechanism, such as conduction tissue disease, which would explain the benefit derived from a pacemaker. It should be recalled that the trials with most favorable results for pacing were those in older patients (60 years in VASIS19 and 58 years in SYDIT20).
There is thus a lack of data concerning the possible benefits of ILRs and subsequent pacemaker implantation in patients with the same characteristics as in ISSUE-3 but aged <40 years.
ConclusionAlthough reflex vasovagal syncope is a relatively benign condition, it has an extremely negative impact on a minority of patients. Pacemaker therapy has gained new impetus in the light of the most recent studies. However, considering the not insignificant complications associated with pacing, it should be considered only in patients aged >40 years, with severe recurrent syncope, in whom long asystoles have been documented with an ILR.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Sousa PA, Candeias R, Marques N, et al. Síncope reflexa vasovagal – haverá benefício da terapêutica com pacemaker? Rev Port Cardiol. 2014;33:297–303.