Familial amyloid polyneuropathy (FAP) is a rare disease caused by systemic deposition of amyloidogenic variants of the transthyretin (TTR) protein. The TTR-V30M mutation is caused by the substitution of valine by methionine at position 30 and mainly affects the peripheral and autonomic nervous systems. Cardiovascular manifestations are common and are due to autonomic denervation and to amyloid deposition in the heart. Cardiac sympathetic denervation detected by iodine-123 labeled metaiodobenzylguanidine (MIBG) is an important prognostic marker in TTR-V30 M FAP. Liver transplantation, widely used to halt neurological involvement, appears to have a varying effect on the progression of amyloid cardiomyopathy. Its effect on the progression of cardiac denervation remains unknown.
MethodsIn this observational study, patients with the TTR-V30 M mutation underwent annual cardiac assessment and serial MIBG imaging with quantification of the late heart-to-mediastinum (H/M) ratio.
ResultsWe studied 232 patients (median age 40 years, 54.7% female, 37.9% asymptomatic at the time of inclusion) who were followed for a median of 4.5 years and underwent a total of 558 MIBG scans. During follow-up, 47 patients (20.3%) died. MIBG scintigraphy at inclusion was a strong predictor of prognosis, with the risk of death increasing by 27.8% for each one-tenth reduction in the late H/M ratio. The late H/M ratio decreased with age (0.082/year, p<0.001), but progression of cardiac denervation was so slow that annual repetition of MIBG imaging did not increase its prognostic accuracy. During follow-up, 70 symptomatic patients underwent liver transplantation. The late H/M ratio decreased by 0.19/year until transplantation but no statistically significant differences were detected after the procedure.
ConclusionsCardiac denervation is common during the progression of TTR-V30 M FAP and quantification of the late H/M ratio on MIBG scintigraphy is valuable for prognostic stratification of these patients. Liver transplantation stabilizes cardiac denervation, without recovery or further deterioration in cardiac MIBG uptake after the procedure.
A polineuropatia amiloidótica familiar (PAF) é uma doença rara devida à deposição sistémica de variantes amiloidogénicas da proteína transtirretina (TTR-V30M), atingindo especialmente o sistema nervoso periférico. As manifestações cardiovasculares são muito comuns e devem-se à desnervação autonómica e à deposição de amiloide no coração. A desnervação simpática cardíaca, detetada por cintigrafia com metaiodobenzilguanidina (MIBG) marcada com I123, é um importante estratificador prognóstico na PAF TTR-V30M. O transplante hepático, amplamente utilizado para interromper a progressão do envolvimento neurológico, parece ter impacto heterogéneo na evolução da miocardiopatia amiloidótica. O seu impacto na progressão da desnervação cardíaca permanece desconhecido.
MétodosEstudo observacional de portadores da mutação TTR-V30M submetidos a avaliação cardiológica anual e a cintigrafias com MIBG seriadas, com quantificação do índice de captação coração/mediastino (C/M) tardio.
ResultadosForam estudados 232 doentes (idade mediana de 40 anos, 54,7% do sexo feminino, 37,9% assintomáticos aquando da inclusão), seguidos durante uma mediana de 4,5 anos e submetidos a um total de 558 cintigrafias MIBG. Durante o seguimento, 47 doentes (20,3%) morreram. A cintigrafia com MIBG inicial foi um forte preditor prognóstico, detetando-se aumento do risco de morte em 27,8% por cada redução decimal do índice C/M tardio. O índice C/M tardio diminuiu com a idade (0,082 por ano; p<0,001), mas a progressão da desnervação cardíaca foi tão lenta que a repetição anual do exame não aumentou a sua precisão prognóstica. Durante o seguimento, 70 doentes sintomáticos foram submetidos a transplante hepático. O índice C/M tardio diminuiu 0,19/ano até ao transplante, deixando de ser detetadas variações estatisticamente significativas a partir do procedimento.
ConclusãoA desnervação cardíaca é frequente durante a progressão da PAF TTR-V30M e a quantificação do índice C/M tardio por cintigrafia MIBG é valiosa para a estratificação prognóstica destes doentes. O transplante hepático permite a estabilização da desnervação cardíaca, não havendo recuperação ou deterioração adicional da captação cardíaca de MIBG após o procedimento.
Familial amyloid polyneuropathy (FAP) due to a mutation in the transthyretin (TTR) protein, in which most frequently valine is replaced by methionine in position 30 (TTR-V30 M), is a multisystem hereditary disease characterized by progressive involvement of sensory, motor and autonomic nerve fibers.1,2 Neurological manifestations are the main clinical feature, but cardiovascular involvement due to autonomic neuropathy and cardiac amyloid deposition is also common.3
Myocardial scintigraphy with iodine-123 labeled metaiodobenzylguanidine (123I-MIBG) is a non-invasive method for quantifying cardiac sympathetic innervation. Previous studies have demonstrated that myocardial sympathetic innervation as detected by 123I-MIBG is decreased in the initial stages of FAP4,5 and that reduction in the late heart-to-mediastinum (H/M) ratio is an important predictor of prognosis that is strongly associated with long-term risk of mortality.6 However, the progression of cardiac denervation during the clinical course of TTR-V30 M FAP has never been assessed by serial 123I-MIBG scans, and the added value of repeated measurement of late H/M for prognostic stratification is unknown.
Liver transplantation is widely used to slow the progression of FAP and until recently was the only treatment option for these patients.7 Transplantation halts neurological involvement and improves survival, especially if performed early in the symptomatic stages of the disease.6 However, amyloid deposition in the heart may continue after transplantation, leading to progressive myocardial thickening, arrhythmias and conduction disturbances.8–13 Little is known of the course of cardiac denervation following liver transplantation.
The aim of this study was to assess the effect of liver transplantation on the progression of cardiac denervation in patients with TTR-V30 M FAP.
MethodsThis was a prospective observational study of consecutive patients with the TTR-V30 M mutation. All subjects underwent annual cardiac assessment and periodic measurement of the late H/M ratio. Progression of cardiac denervation was determined by comparing the H/M ratio in successive exams.
123I-MIBG scintigraphy was performed following premedication with Lugol's solution (iodine-potassium iodide) to block absorption of free 123I by the thyroid gland. Chronic medication was not suspended before the exam. Planar anterior thoracic images were acquired 15 min (early) and 3 h (late) after intravenous injection of a fixed dose of 185 MBq of 123I-MIBG. A dual-head gamma camera (Millennium, General Electric Healthcare) equipped with a low-energy, high-resolution parallel-hole collimator was used for image acquisition and a 20% energy window was centered over the 159keV photopeak of 123I.
123I-MIBG uptake was quantified through the H/M ratio, which was calculated by dividing the mean counts per pixel in the region of interest around the heart by the mean counts per pixel in the mediastinum, without correction for background activity. The myocardial washout rate was calculated as the percentage reduction of myocardial counts between early and late images:
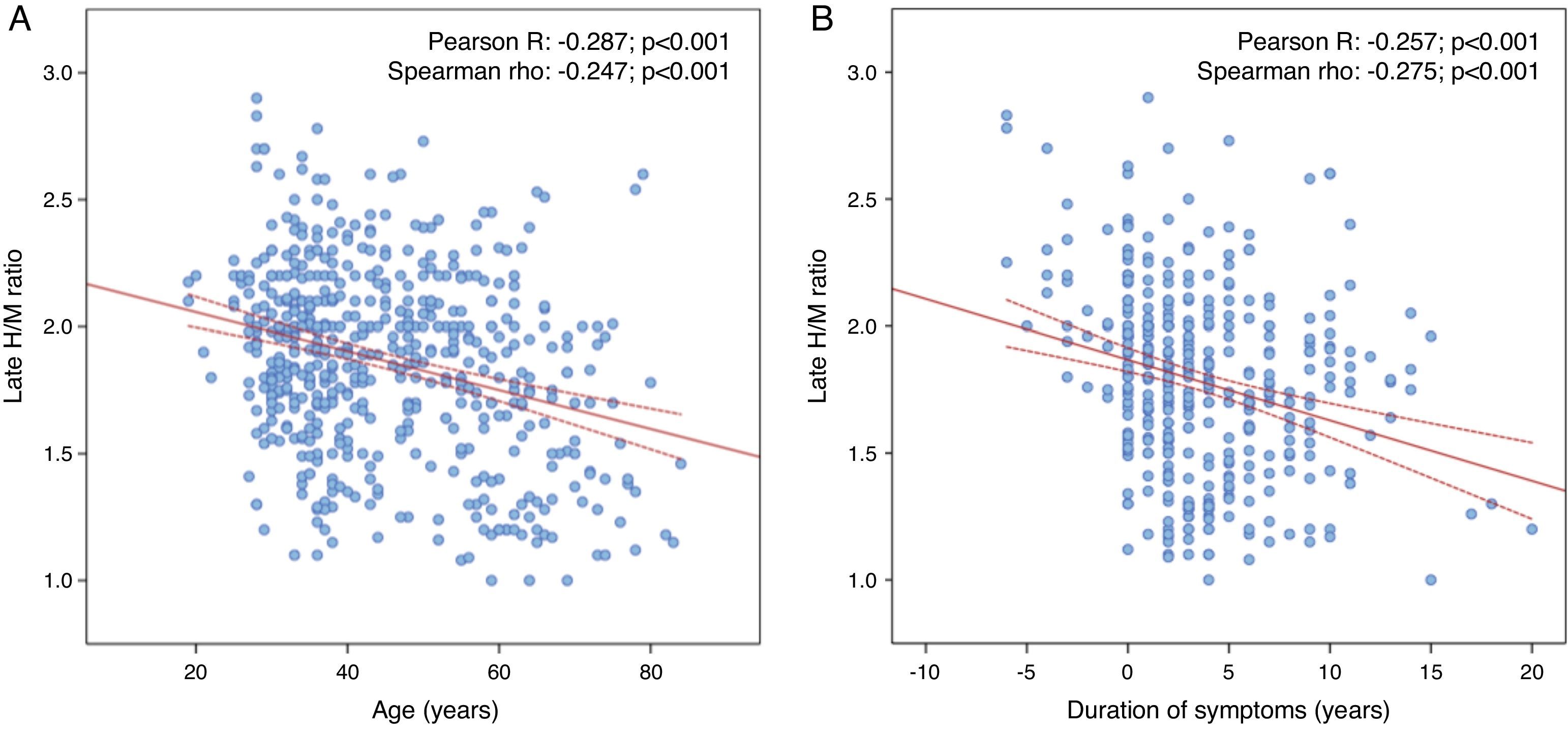
Statistical analysisContinuous variables with normal distribution were expressed as means±standard deviation and were compared using the Student's t test or analysis of variance, and those with non-normal distribution were expressed as medians and interquartile range (IQR) and compared with the Mann-Whitney or Kruskal-Wallis tests. Scintigraphic parameters were correlated with age, duration of symptoms and time before and after liver transplantation, using Pearson's and Spearman's correlation coefficients.
The prognostic impact of scintigraphic parameters on all-cause mortality during follow-up was determined by Cox univariate and multivariate regression analysis adjusted for age. To avoid bias, stepwise methods were used for the multivariate analysis, with non-significant variables being removed from the model at each step (p-value 0.05 for inclusion and 0.10 for removal). The accuracy of predictors of mortality was assessed by the area under the curve (AUC) on receiver operating characteristic analysis for different durations of follow-up. Cumulative event rates by quartiles of H/M ratio were assessed by the Kaplan-Meier method and the log-rank test.
The statistical analysis was performed with SPSS version 21.0 (IBM SPSS, Chicago, IL). A p-value <0.05 was considered statistically significant.
ResultsPopulation characteristicsBetween September 1998 and July 2015, 305 carriers of the TTR-V30 M mutation underwent annual cardiac assessment. A total of 73 patients were excluded from the analysis: 45 for not having undergone MIBG imaging and 28 because their first MIBG scan was performed after liver transplantation. The final study population thus consisted of 232 patients, median age 40 years (IQR 32-55), 54.7% female (n=127).
At the initial cardiac assessment, 144 patients (62.1%) had documented neurological involvement, the other 88 (37.9%) being asymptomatic. Of the symptomatic patients, 99 had developed clinical manifestations by the age of 50, while the other 45 had late onset (after the age of 50). The mean age of symptom onset was 38 years (IQR 31-54) and the mean duration of symptoms at initial assessment was two years (IQR 0-3). Nineteen carriers of the pathogenic mutation aged over 50 were still symptom-free.
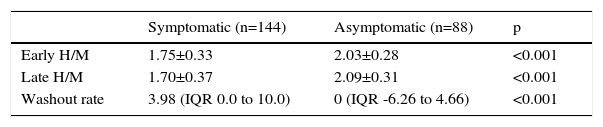
123I-MIBG scintigraphyAt the initial assessment, the mean early and late H/M ratios were 1.85±0.23 and 1.83±0.03, respectively, and median washout rate was 2.5 (IQR -2.3 to 8.5). Early and late H/M ratios were significantly lower and the washout rate was significantly higher in symptomatic patients (Table 1).
Comparison of scintigraphic parameters according to neurological involvement.
| Symptomatic (n=144) | Asymptomatic (n=88) | p | |
|---|---|---|---|
| Early H/M | 1.75±0.33 | 2.03±0.28 | <0.001 |
| Late H/M | 1.70±0.37 | 2.09±0.31 | <0.001 |
| Washout rate | 3.98 (IQR 0.0 to 10.0) | 0 (IQR -6.26 to 4.66) | <0.001 |
H/M: heart-to-mediastinum ratio; IQR: interquartile range.
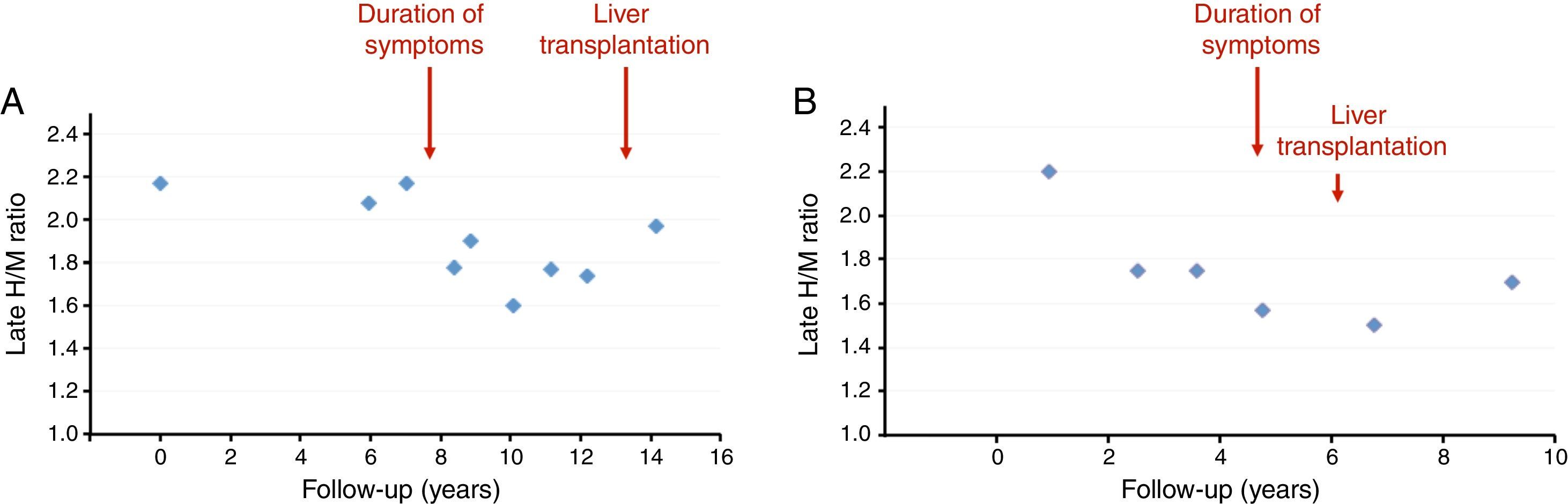
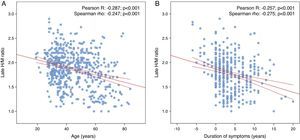
During a median follow-up of 4.5 years (IQR 2.1-7.7; maximum 15.6), 121 patients underwent serial MIBG imaging, of whom 36 underwent at least five exams (maximum nine) (Supplementary Table 1). Including both initial and subsequent assessments, a total of 558 MIBG scans were performed. In these exams, the late H/M ratio decreased with age (by 0.082/year, p<0.001) and with duration of symptoms (by 0.066/year, p<0.001) (Figure 1 and Supplementary Table 2), to a similar degree in both sexes (Supplementary Figure 1). Figure 2 presents the progression of late H/M in serial MIBG scans of two typical patients, illustrating the slow reduction in the presymptomatic stage of the disease, the more marked decline after symptom onset, and the apparent stabilization after liver transplantation.
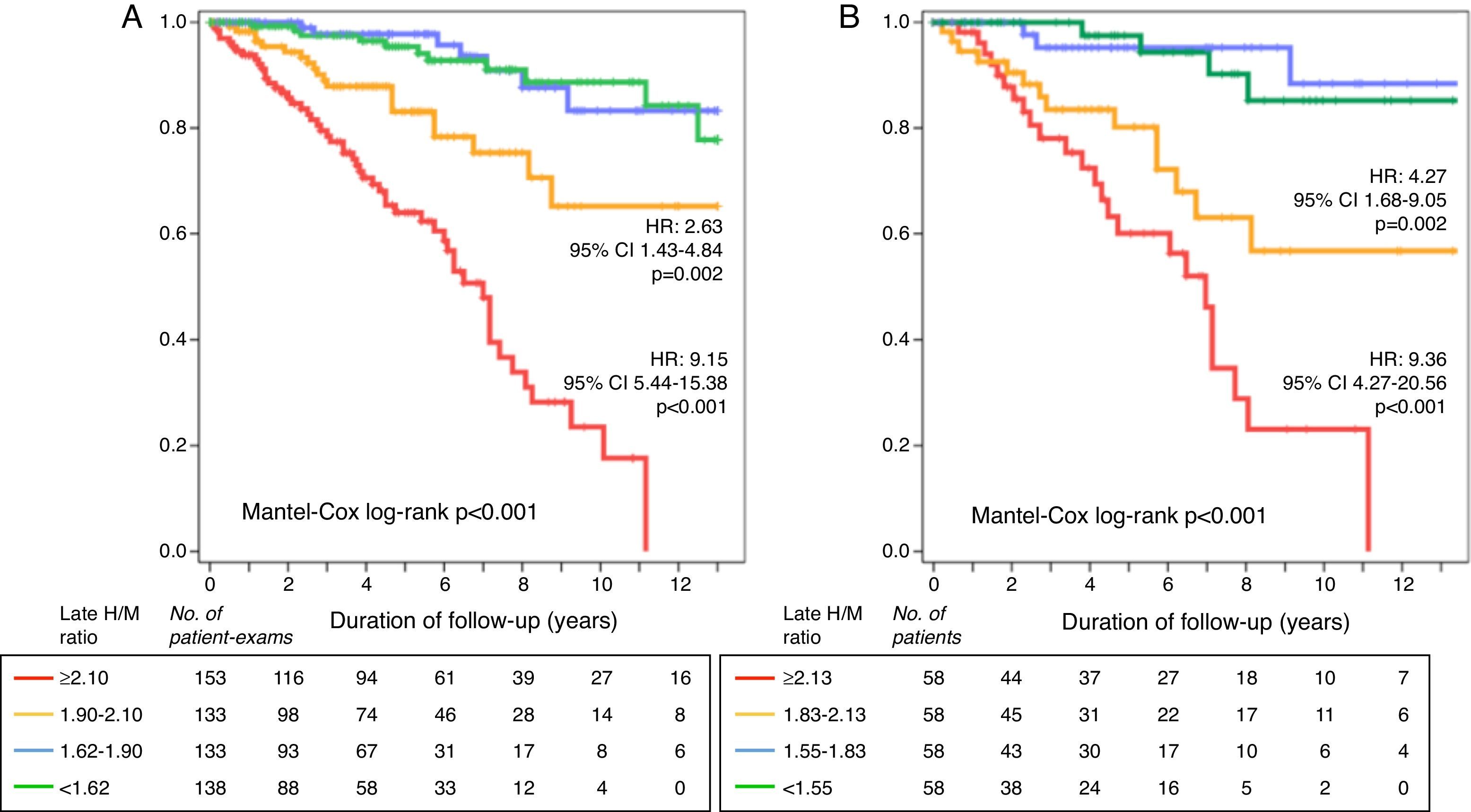
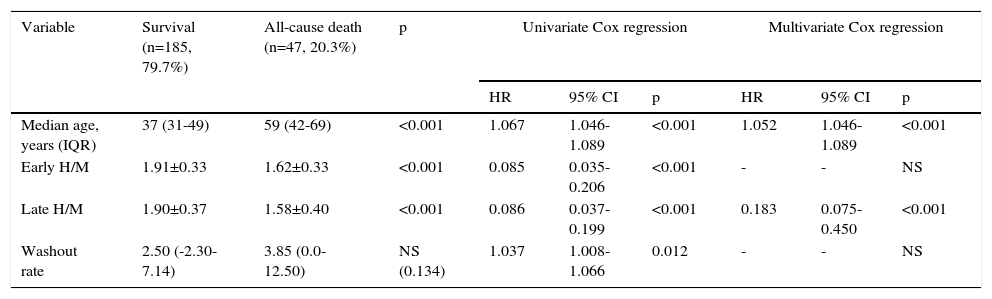
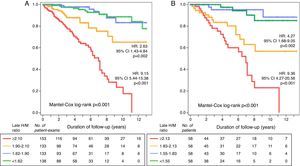
During follow-up, 47 patients (20.3%) died. The most frequent cause of death (40%) was terminal FAP (Supplementary Table 3). MIBG scintigraphy at inclusion was a strong predictor of prognosis, with the risk of death increasing by 27.8% (95% confidence interval [CI] 17.5-39.1) for each one-tenth reduction in the late H/M ratio (hazard ratio [HR] 0.78; 95% CI 0.72-0.85; p<0.001). Of the MIBG parameters, only late H/M was an independent prognostic predictor (Table 2). Mortality was nine times higher in patients with lower H/M (first quartile, <1.55) at inclusion than in those with H/M above the median for the study population (≥1.83; HR 9.36; 95% CI 4.27-20.56; p<0.001). Mortality was also four times higher in patients with moderate reductions (1.55-1.83) in late H/M (HR 4.27; 95% CI 1.68-9.05; p=0.002) (Figure 3A).
Mortality during follow-up by age and MIBG parameters at inclusion.
| Variable | Survival (n=185, 79.7%) | All-cause death (n=47, 20.3%) | p | Univariate Cox regression | Multivariate Cox regression | ||||
|---|---|---|---|---|---|---|---|---|---|
| HR | 95% CI | p | HR | 95% CI | p | ||||
| Median age, years (IQR) | 37 (31-49) | 59 (42-69) | <0.001 | 1.067 | 1.046-1.089 | <0.001 | 1.052 | 1.046-1.089 | <0.001 |
| Early H/M | 1.91±0.33 | 1.62±0.33 | <0.001 | 0.085 | 0.035-0.206 | <0.001 | - | - | NS |
| Late H/M | 1.90±0.37 | 1.58±0.40 | <0.001 | 0.086 | 0.037-0.199 | <0.001 | 0.183 | 0.075-0.450 | <0.001 |
| Washout rate | 2.50 (-2.30-7.14) | 3.85 (0.0-12.50) | NS (0.134) | 1.037 | 1.008-1.066 | 0.012 | - | - | NS |
CI: confidence interval; H/M: heart-to-mediastinum ratio; HR: hazard ratio; IQR: interquartile range; NS: non-significant.
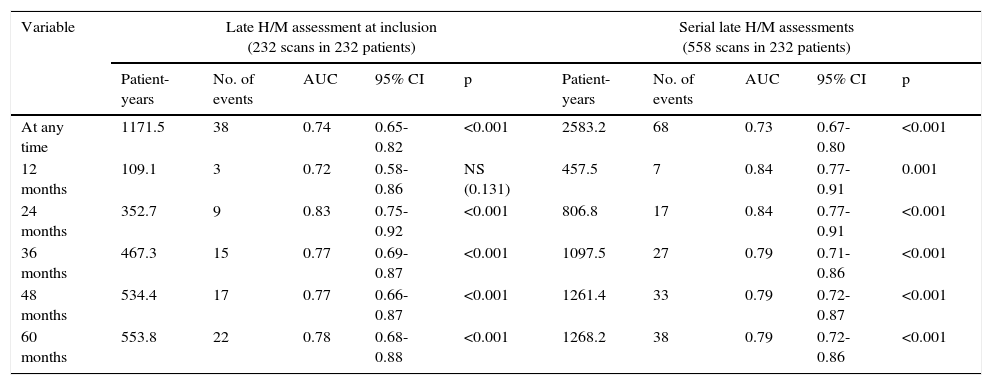
To determine the potential added value of serial late H/M assessment for prognostic stratification, we assessed the accuracy of all the MIBG scans (558 scans, 2246 patient-years of follow-up) for predicting post-exam survival, which was found to be significantly reduced with lower late H/M ratio. The risk of death increased by 27.8% for every one-tenth reduction in the late H/M ratio (HR 0.774; 95% CI 0.73-0.82; p<0.001), and was nine times higher in patients in the first H/M quartile (HR 9.15; 95% CI 5.44-15.38; p<0.001) (Figure 3B).
The accuracy of prediction based on serial exams was assessed by the area under the curve (AUC) on receiver operating characteristic analysis for different time intervals and compared with prognostic stratification based only on the initial MIBG scan (Table 3). Prognostic stratification based on annual repetition of MIBG imaging was slightly superior, but the differences were trivial for time intervals less than the median follow-up (4.5 years). The statistical power of prognostic stratification based on a single exam and on serial exams was similar, and very high (99%).
Accuracy of initial and serial late H/M ratios in MIBG scans for predicting mortality assessed by receiver operating characteristic analysis.
| Variable | Late H/M assessment at inclusion (232 scans in 232 patients) | Serial late H/M assessments (558 scans in 232 patients) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Patient-years | No. of events | AUC | 95% CI | p | Patient-years | No. of events | AUC | 95% CI | p | |
| At any time | 1171.5 | 38 | 0.74 | 0.65-0.82 | <0.001 | 2583.2 | 68 | 0.73 | 0.67-0.80 | <0.001 |
| 12 months | 109.1 | 3 | 0.72 | 0.58-0.86 | NS (0.131) | 457.5 | 7 | 0.84 | 0.77-0.91 | 0.001 |
| 24 months | 352.7 | 9 | 0.83 | 0.75-0.92 | <0.001 | 806.8 | 17 | 0.84 | 0.77-0.91 | <0.001 |
| 36 months | 467.3 | 15 | 0.77 | 0.69-0.87 | <0.001 | 1097.5 | 27 | 0.79 | 0.71-0.86 | <0.001 |
| 48 months | 534.4 | 17 | 0.77 | 0.66-0.87 | <0.001 | 1261.4 | 33 | 0.79 | 0.72-0.87 | <0.001 |
| 60 months | 553.8 | 22 | 0.78 | 0.68-0.88 | <0.001 | 1268.2 | 38 | 0.79 | 0.72-0.86 | <0.001 |
AUC: area under the curve on receiver operating characteristic analysis. All other abbreviations as in Table 2.
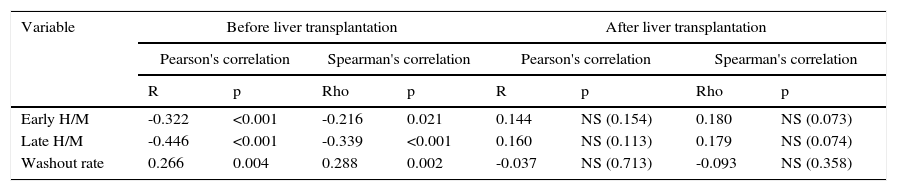
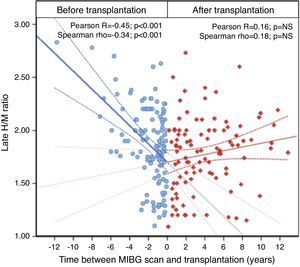
Seventy patients (30.2%) underwent liver transplantation. In 39 of these patients surgery was performed less than one year after initial assessment. Perioperative mortality was 7.1% (5/70). The effect of transplantation on progression of sympathetic denervation was determined by comparing reductions in the late H/M ratio in images before (116 exams) and after (100 exams) transplantation. Of the former, 53 were performed less than a year before surgery.
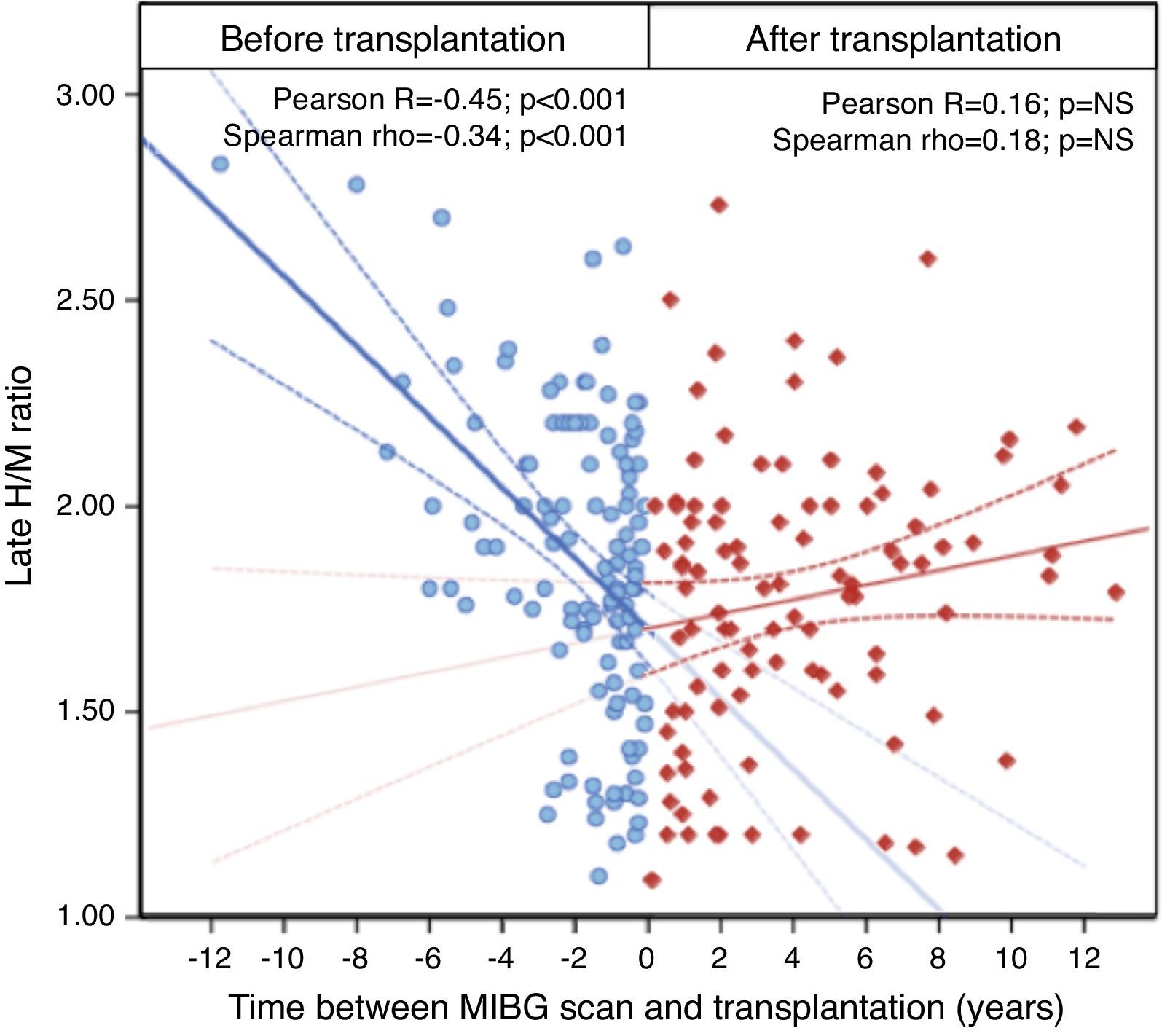
In symptomatic patients requiring transplantation, late H/M decreased by 0.19/year (p<0.001) until transplantation; early H/M also decreased progressively and the MIBG washout rate increased. By contrast, all scintigraphic parameters stabilized after transplantation and no statistically significant differences were detected over time (Table 4 and Figure 4).
Correlations between scintigraphic parameters and time before and after liver transplantation.
| Variable | Before liver transplantation | After liver transplantation | ||||||
|---|---|---|---|---|---|---|---|---|
| Pearson's correlation | Spearman's correlation | Pearson's correlation | Spearman's correlation | |||||
| R | p | Rho | p | R | p | Rho | p | |
| Early H/M | -0.322 | <0.001 | -0.216 | 0.021 | 0.144 | NS (0.154) | 0.180 | NS (0.073) |
| Late H/M | -0.446 | <0.001 | -0.339 | <0.001 | 0.160 | NS (0.113) | 0.179 | NS (0.074) |
| Washout rate | 0.266 | 0.004 | 0.288 | 0.002 | -0.037 | NS (0.713) | -0.093 | NS (0.358) |
Abbreviations as in Table 2.
In this large prospective study of carriers of the TTR-V30 M mutation followed for a median of 4.5 years, we analyzed the progression of cardiac sympathetic denervation as assessed by the H/M MIBG uptake ratio, the prognostic value of this index for long-term survival, and the effect of liver transplantation. The main results are as follows: (1) cardiac denervation progresses slowly in the pre-symptomatic stages of the disease but tends to accelerate after symptom onset; (2) MIBG scintigraphy at inclusion is a strong predictor of prognosis, with the risk of death increasing by 27.8% for each one-tenth reduction in the late H/M ratio; and (3) liver transplantation stabilizes cardiac denervation in long-term follow-up.
The cardiovascular manifestations of TTR-V30 M FAP are caused by autonomic dysfunction (disrupted control of blood pressure and heart rate) and by cardiac amyloid deposition (infiltrative cardiomyopathy, arrhythmias and conduction disturbances). However, phenotypic differences are seen in TTR-V30 M carriers according to geographic origin: cohort studies of Swedish patients report a high prevalence of restrictive cardiomyopathy,3,14 which is rare in Portugal, where cardiac autonomic neuropathy and conduction disturbances tend to dominate the clinical picture.6
Previous studies have shown that MIBG scintigraphy is an indirect way to visualize the impairment of cardiac sympathetic innervation by amyloid deposition. Nakata et al.15 were the first to report a case of a patient with TTR-V30 M FAP with no myocardial activity on MIBG imaging, indicating involvement of the sympathetic nerves. Subsequent small studies demonstrated not only that myocardial denervation was strongly correlated with severity of polyneuropathy16 but also that MIBG uptake may be reduced before the onset of clinically apparent cardiac disease.5 In a previous study of 143 individuals, we showed that cardiovascular abnormalities as assessed by electrocardiography, Holter monitoring, ambulatory blood pressure monitoring, echocardiography and MIBG scintigraphy are common in TTR-V30 M FAP, particularly in patients with neurological involvement.6 Unlike other forms of systemic amyloidosis, the cardiovascular involvement in our study was mostly subclinical and obvious cardiac manifestations were rare. However, we did find that subclinical cardiovascular manifestations often preceded neurological involvement, which offers the possibility of earlier recognition of the onset of disease in asymptomatic carriers. We also demonstrated the prognostic value of MIBG imaging, which was in fact the strongest prognostic predictor of all the cardiac and neurological parameters assessed: patients with late H/M of less than 1.60 had a seven-fold higher risk of death during follow-up.
The present study confirms previous findings in a larger population and broadens the results to include serial H/M assessments. As expected, late H/M decreased significantly over time, but progression of cardiac denervation was so slow that annual repetition of MIBG imaging did not increase its accuracy in predicting all-cause death. Our results therefore suggest that repeated assessment of the H/M ratio is not justified for the purposes of prognostic stratification, at least not more often than at intervals of less than five years (the median duration of follow-up in the present study).
Liver transplantation has been widely used for the last twenty years to remove the main source of mutant transthyretin, in order to slow the progression of clinical manifestations, including peripheral neuropathy, gastrointestinal symptoms and other visceral complications.7,17–20 Transplantation also improves long-term survival, especially when performed in the early stages of symptomatic disease.6,21 However, the effect of liver transplantation on the progression of cardiomyopathy in TTR-V30 M FAP is the subject of debate, with some studies suggesting that transplanted patients do not develop overt cardiomyopathy,22,23 while others – in Swedish,10,13 French12 and Japanese9 patients – report progression of arrhythmias and myocardial thickening due to amyloid deposition. This adverse outcome appears to be more frequent in Swedish patients with late-onset TTR-V30 M FAP.3,10,13
It has been suggested that the main component of cardiac amyloid deposits following liver transplantation is normal (wild-type) transthyretin.24 Nevertheless, none of the studies that monitored the progression of amyloid infiltration by echocardiography following liver transplantation assessed its effect on cardiac autonomic denervation. In a small group of 31 French patients, Delahaye et al.12 compared the H/M ratio before and after liver transplantation, complemented with echocardiography; as in our study, no change was seen in sympathetic innervation following transplantation in a short follow-up (24±15 months), even though cardiac amyloid infiltration, as measured by myocardial thickness, had progressed. In the present study, of a larger group (70) of transplanted patients, the rate of decrease in H/M was assessed by comparing MIBG scintigraphy before (116 exams) and after (100 exams) transplantation. Of note, all scintigraphic parameters stabilized after surgery. There thus appears to be a distinction between amyloid deposition as assessed by myocardial thickness on echocardiography, which may progress after transplantation, and autonomic nerve involvement, which tends to stabilize.
ConclusionsCardiac denervation is common during the progression of TTR-V30 M FAP and quantification of the late H/M ratio on MIBG scintigraphy is valuable for prognostic stratification of these patients. Liver transplantation stabilizes cardiac denervation. Following transplantation, cardiac 123I-MIBG uptake remains stable over time, with no further recovery or deterioration. It is thus essential to perform transplantation sufficiently early in the natural history of the disease.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Azevedo Coutinho MdC, Cortez-Dias N, Cantinho G, Conceição I, Guimarães T, Lima da Silva G, et al. Progressão da desnervação simpática cardíaca avaliada por cintigrafia com MIBG-I123 na polineuropatia amiloidótica familiar e o impacto da transplantação hepática. Rev Port Cardiol. 2017;36:333–340.