Primary cardiac lymphoma is defined as non-Hodgkin lymphoma involving the heart and/or pericardium. It is a rare cancer that primarily affects the right heart and in particular the right atrium. By contrast, renal cell carcinoma is a relatively common cancer, which in rare circumstances can metastasize to the heart. It is now known that there is an association between non-Hodgkin lymphoma and renal cell carcinoma, although the underlying mechanisms are not fully understood. The authors present a case of primary cardiac non-Hodgkin lymphoma in a patient with concomitant renal cell carcinoma and explore the possible reasons for this association.
O linfoma primário do coração é definido como um linfoma não Hodgkin que envolve o coração e/ou o pericárdio. Trata-se de uma neoplasia rara que envolve principalmente as cavidades direitas e, em especial, a aurícula direita. Por sua vez, o carcinoma das células renais é uma neoplasia relativamente comum que, em situações mais raras, pode metastizar para o coração. Atualmente, é conhecida uma associação entre a ocorrência de linfomas não Hodgkin e de carcinomas das células renais, apesar dos mecanismos a ela subjacentes não serem claramente conhecidos. Com este artigo, os autores apresentam um caso de um linfoma não Hodgkin primário do coração num doente com uma neoplasia renal síncrona e exploram as bases admitidas para esta associação.
Non-Hodgkin lymphoma (NHL) is associated with a higher incidence of other cancers, both solid tumors and other blood cancers. Studies by Travis et al.1,2 showed a high probability of a second cancer in NHL patients, increasing over time. The incidence of renal cell carcinoma (RCC) appears to be particularly high in these patients, with a reported observed-to-expected ratio of 1.47–2.07.1,2
The explanations initially proposed for this association were the late effects of chemotherapy and radiation therapy used in cancer treatment or immunosuppression caused by the disease itself. While this may be true of certain cancers such as leukemia and bladder cancers, which are frequently associated with previous use of alkylating agents, it does not explain why some of these cancers precede lymphoma or develop in patients who have not undergone treatment with these agents.1,2
However, other studies have found a higher than expected incidence of RCC in NHL patients based on the incidence of each disease in the general population. A study by Anderson et al.3 found concomitant RCC and NHL in 41 patients. The data from this study showed that NHL patients have a relative risk of 1.86 of developing RCC, while RCC patients have a relative risk of 2.67 of developing NHL, similarly to other studies.3–5 We present a case report of primary cardiac lymphoma in a patient with concomitant RCC, which highlights the importance of this association.
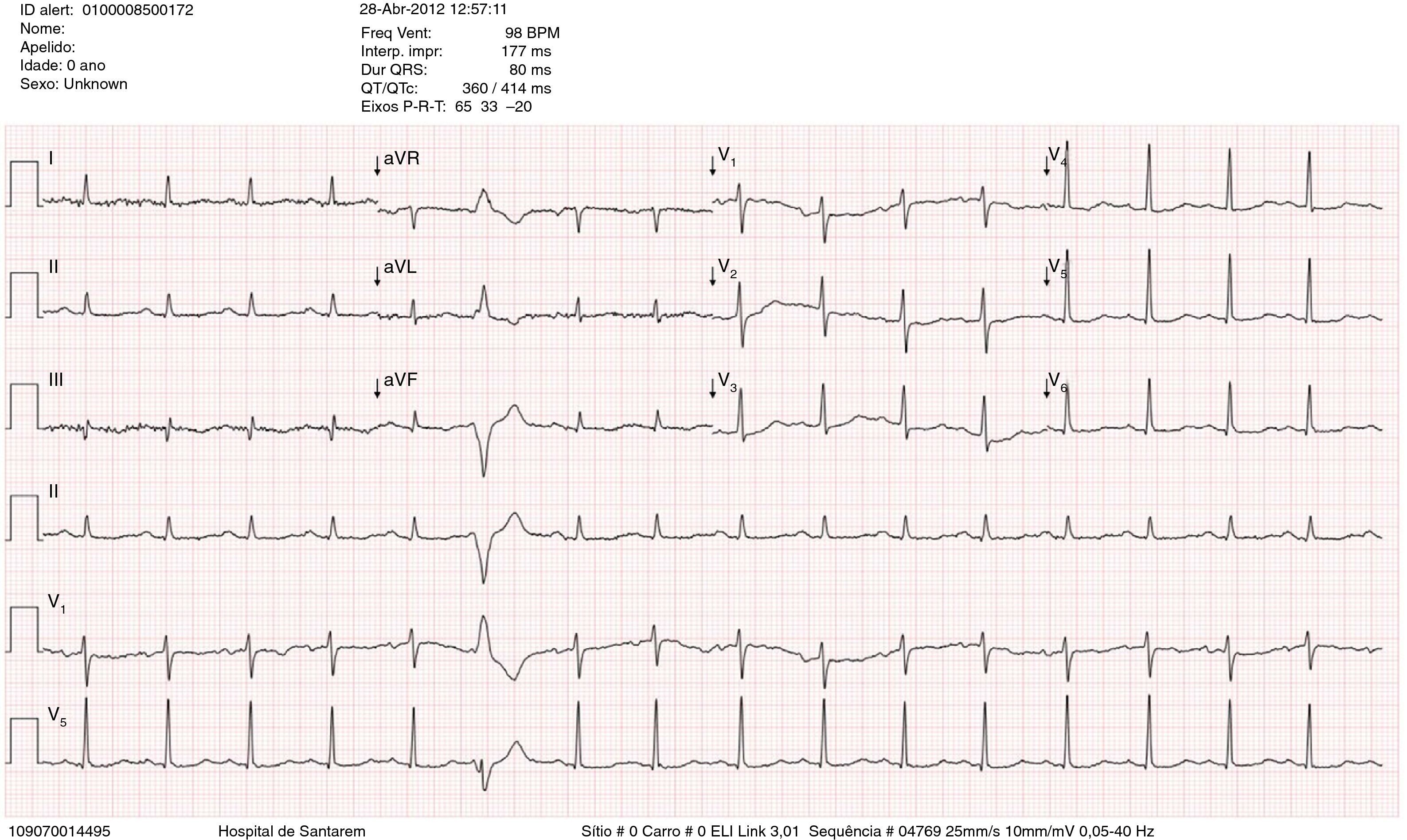
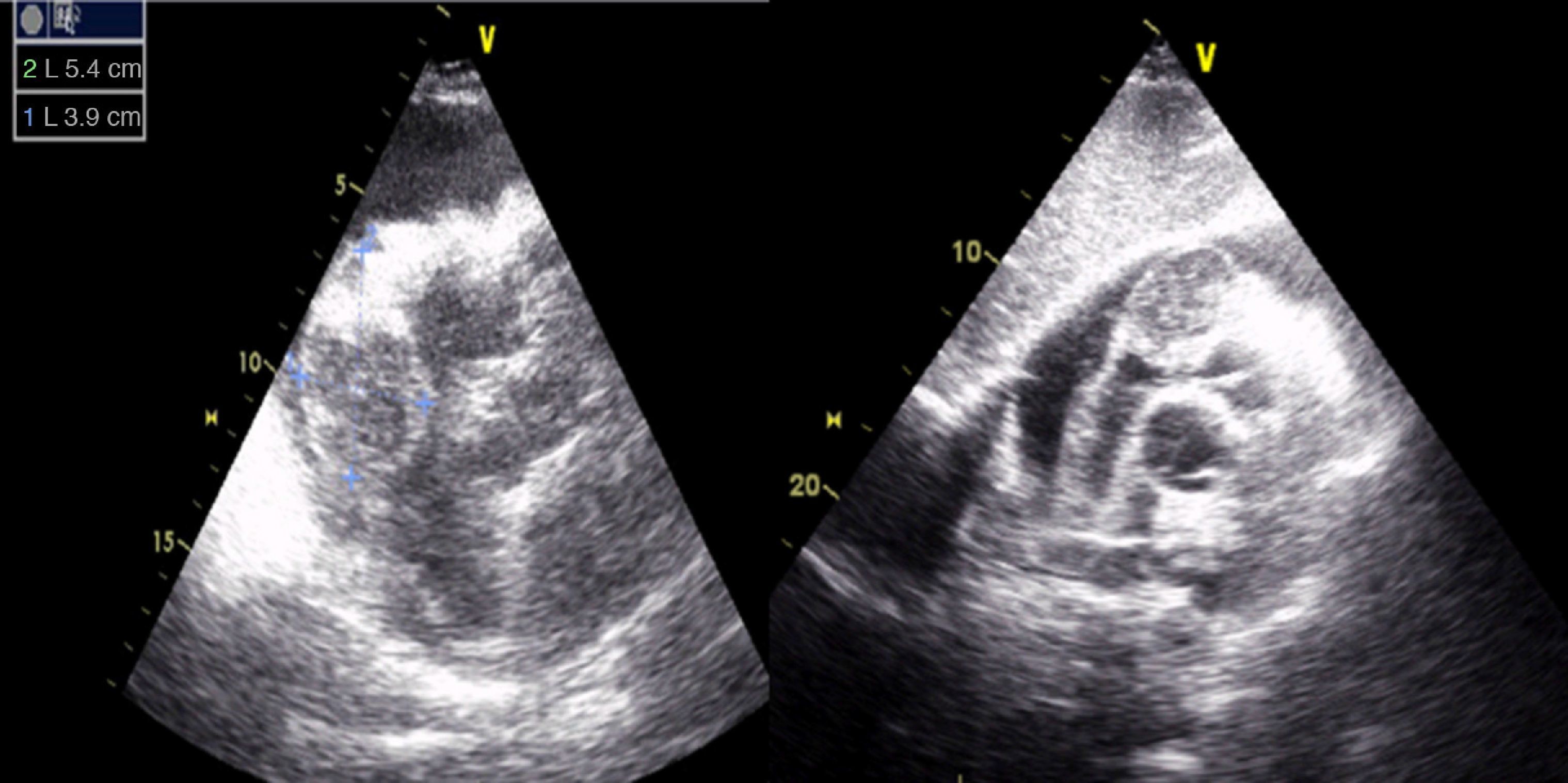
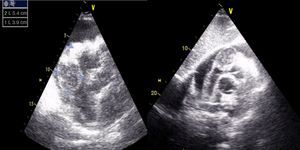
Case reportA 67-year-old man, white, with a history of hypertension and dyslipidemia, went to the emergency department due to increasing fatigue over the previous two weeks, epigastric discomfort radiating to the retrosternal region, and weight loss (around 3 kg in two weeks). He denied fever, cough, expectoration, dyspnea or limb edema. On physical examination, he was hemodynamically stable and apyretic but became short of breath on minimal exertion (28 cpm). Heart sounds were muffled but there was no peripheral edema. The electrocardiogram (ECG) showed sinus tachycardia with low voltage QRS in the limb leads (Figure 1). Laboratory tests revealed slightly elevated creatinine (1.5 mg/dl) and markedly elevated BNP (3462 pg/dl), no increase in inflammatory markers (leukocytes 4.9×109/l and C-reactive protein 3.9 mg/dl), hemoglobin 13.9 g/dl, and negative markers of myocardial necrosis. The echocardiogram showed a large circumferential pericardial effusion and an oval, heterogeneous mass at the level of the right atrioventricular groove, together with thickening of the right ventricular free wall (Figure 2).
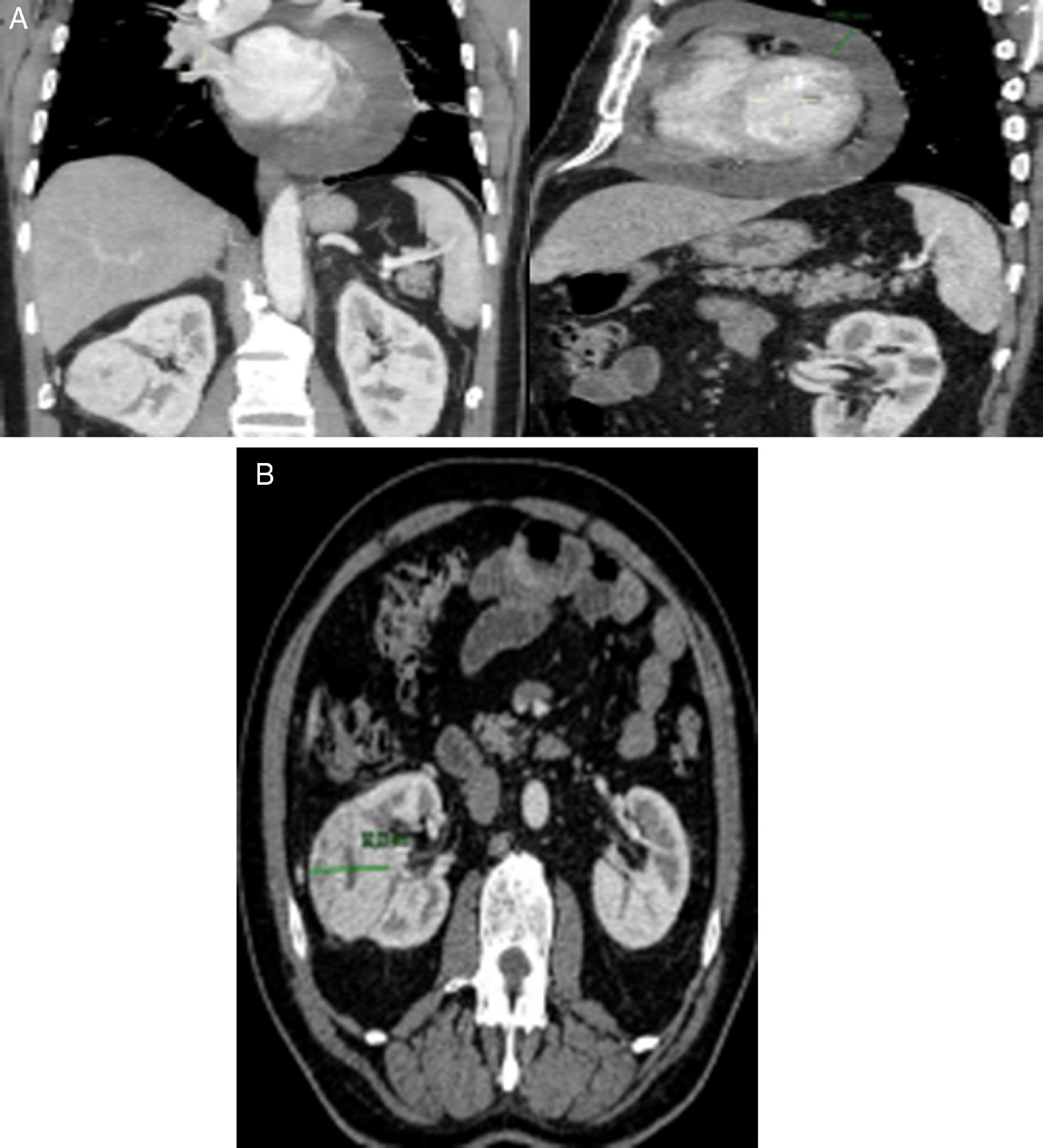
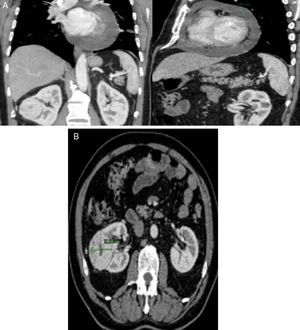
Thoracic-abdominal-pelvic computed tomography (CT) was performed to characterize the pericardial effusion and cardiac mass and to exclude associated cancer. This confirmed a lesion with contrast uptake in the vicinity of the right atrium (Figure 3A), together with a solid, nodular lesion in the right kidney suggestive of RCC (Figure 3B). Cardiac and abdominal magnetic resonance imaging (MRI) was also performed, which was inconclusive as to whether the cardiac lesion was primary or secondary but which confirmed the suspicion of primary renal cancer.
The patient underwent right nephrectomy and anatomopathological study confirmed that the kidney lesion was conventional RCC, Fuhrman grade 2, with no evidence of extrarenal involvement.
Given the discrepancy between the absence of local involvement of the kidney lesion and the presence of a cardiac mass that could be a secondary lesion, it was decided to refer the patient for heart biopsy; the result of anatomopathological study was consistent with diffuse CD20+ large B cell NHL.
Following confirmation of the diagnosis, the patient was referred to the hematology clinic, where he began chemotherapy, with partial clinical response and stabilization of the disease after the second treatment cycle.
DiscussionPrimary cardiac lymphoma is defined as NHL involving the heart and/or the pericardium. In contrast to cardiac involvement in diffuse NHL, which occurs in up to 20% of patients, primary cardiac lymphoma is a rare entity, accounting for 1.3% of all primary cardiac tumors and 0.5% of all extranodal lymphomas.6
There is no pathognomonic clinical presentation, symptoms depending on the site of the cancer. Primary cardiac lymphoma primarily affects the right heart and in particular the right atrium, as was the case in our patient.6
The ECG in most cases, including the one presented, shows nonspecific alterations in ventricular repolarization and low voltage QRS complexes, the most common arrhythmia being complete atrioventricular block.7,8
Transthoracic echocardiography is the first-line diagnostic exam as it provides the best images of the right heart, while newer imaging techniques such as CT and MRI are increasingly used to assess these patients due to their excellent spatial resolution.7 As in the case presented, primary cardiac lymphoma tends to present as an isodense or hypodense image, with slow and heterogeneous contrast uptake.9 Pericardial effusion and thickening are also frequent findings.9,10
Approximately 45% of patients with RCC present with localized tumors, as in the case presented, while 30% may have metastases at the time of diagnosis.11 Although the heart may be one of the organs affected, the most common metastatic sites are, in descending order, the lungs, bone, soft tissues, liver and central nervous system.11
Cardiac metastization of neoplasms is rare. A study of 266 cases of neoplasms involving the heart among 11432 autopsies showed that only three originated from renal cancer.12 When it does occur, it tends to present two distinct patterns: isolated involvement of the right heart, often through hematogenous dissemination via the inferior vena cava; or concomitant involvement of the left heart through a lymphatic pathway involving the carinal lymph nodes and parasternal lymph vessels.13 Cardiac involvement in the absence of inferior vena cava thrombi is even rarer.14 The combination of all these findings led us to request a biopsy of the cardiac mass, since there was a high probability of it being a different neoplasm.
As previously mentioned, NHL patients appear to have a higher incidence of RCC. To date no specific mechanism has been established to explain this association, although a number of factors have been proposed, including previous therapy, immune dysfunction, genetic predisposition and environmental factors. Among the most widely discussed are immune dysfunction, a possible viral etiology and genetic predisposition.1,2
According to the hypothesis of immune dysfunction, the immune dysregulation induced by the primary neoplasm predisposes the patient to a second cancer. A study by Yagisawa et al.15 showed the presence of multiple immunological disorders (asthma, idiopathic thrombocytopenic purpura and mesangial proliferative glomerulonephritis) in a patient with NHL and RCC, suggesting an abnormal immunological mechanism. There is also a higher incidence of NHL in patients with melanoma, and the fact that melanoma and RCC respond to immunotherapy suggests immune dysfunction as a possible mechanism.3,16
Certain viruses are now known to be potentially carcinogenic, notably Epstein-Barr virus and human T-lymphotropic virus type 1,17 and a possible viral etiology for certain types of lymphoma has been reported in various studies. Etkind et al.18 detected mouse mammary tumor virus-like DNA sequences in a T-cell lymphoma of a breast cancer patient who was simultaneously diagnosed with both diseases. Subsequent studies by the same group isolated similar viral sequences in lymphomas and breast cancer cells from patients with both diseases.19 Basombrio et al.20 obtained data in an animal model that were consistent with a common viral etiology between NHL and certain solid organ cancers.
The available evidence shows common chromosome abnormalities between RCC and NHL, the most frequent being chromosome 17p deletions and p53 mutations. However, it has yet to be determined whether the same genes are involved in both cancers.21,22
ConclusionPrimary tumors of the heart are rare. Many patients are asymptomatic or present only vague and nonspecific symptoms. Cardiac lymphomas are particularly rapid growing and have a poor short-term prognosis, so early detection is essential.
There has been a steady increase in the number of cases reported of concomitant RCC and NHL, and the association appears to be multifactorial. Genetic predisposition, common immune diseases and environmental factors may all contribute to this association. However, further studies are required to clarify the common etiology of these two cancers.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Severino D, Santos B, Costa C, Durão D, Alves M, Monteiro I, et al. Linfoma primário do coração em doente com neoplasia renal síncrona. Rev Port Cardiol. 2015;34:773.