Functional tricuspid regurgitation is a prevalent disease, especially among patients with other valve disorders, and is associated with significant morbidity and mortality. Its management is challenging, and many patients deemed at high surgical risk are managed conservatively. Despite optimization of pharmacological treatment, many patients continue to be symptomatic, thus leading to interest in percutaneous interventional techniques. The Mitralign system has recently been used for the treatment of functional tricuspid regurgitation, with favorable clinical and imaging results.
We report the first case in Portugal to our knowledge of percutaneous tricuspid regurgitation treatment with the Mitralign system.
A insuficiência tricúspide funcional é uma patologia prevalente, especialmente em doentes com outras valvulopatias, podendo estar associada a importante morbilidade e mortalidade. A sua abordagem é desafiante, sendo que diversos doentes considerados de alto risco cirúrgico são abordados conservadoramente. Apesar do aprimoramento farmacológico, muitos mantêm sintomas, o que leva ao interesse em formas de tratamento percutâneo. O sistema Mitralign foi recentemente usado nesse contexto, com resultados clínicos e imagiológicos favoráveis.
Reportamos aquele que é, no nosso conhecimento, o primeiro caso de tratamento percutâneo de insuficiência tricúspide com o sistema Mitralign, em Portugal.
Tricuspid regurgitation (TR) is a clinical entity with significant prevalence,1,2 and is frequently associated with other valve disorders (especially mitral valve disease).1,3
In western countries, functional (or secondary) TR due to right ventricle (RV) and/or tricuspid annular dilatation in the context of pressure or volume overload (such as left-sided valve disease, pulmonary hypertension or RV dysfunction) is the most common etiology of TR.4,5
Although TR may be well tolerated, particularly in its early stages, progression of the disease often leads to right heart failure.4,6 Contrary to previous conceptions regarding the natural history of TR, contemporary data show that TR may progress after left-sided valve intervention.1,6–8 This is relevant given that, contrary to early tricuspid intervention, re-operation is often associated with a high risk.8
Several studies have also shown that, in different clinical contexts, TR is associated with adverse outcomes, namely mortality.6,9–12
These considerations have led to a new interest in the field of percutaneous intervention in functional TR,4,8 which could provide a new option in high-risk patients. However, challenges concerning the anatomy of the tricuspid valve as well as the impact of hemodynamic factors in its adequate quantification have been important considerations.4–6,8 Different devices have been designed in an attempt to address this issue.8 One such device, the Mitralign system (Mitralign Inc., Tewksbury, Massachusetts), originally developed in the context of functional mitral regurgitation,13 has been successfully implanted in a patient with severe TR.14 This device replicates the Kay procedure, first described over 50 years ago, in which the tricuspid valve is converted into a mitral-like valve after plication of the valve annulus.15
We report the first case in Portugal to our knowledge of percutaneous TR treatment with the Mitralign system.
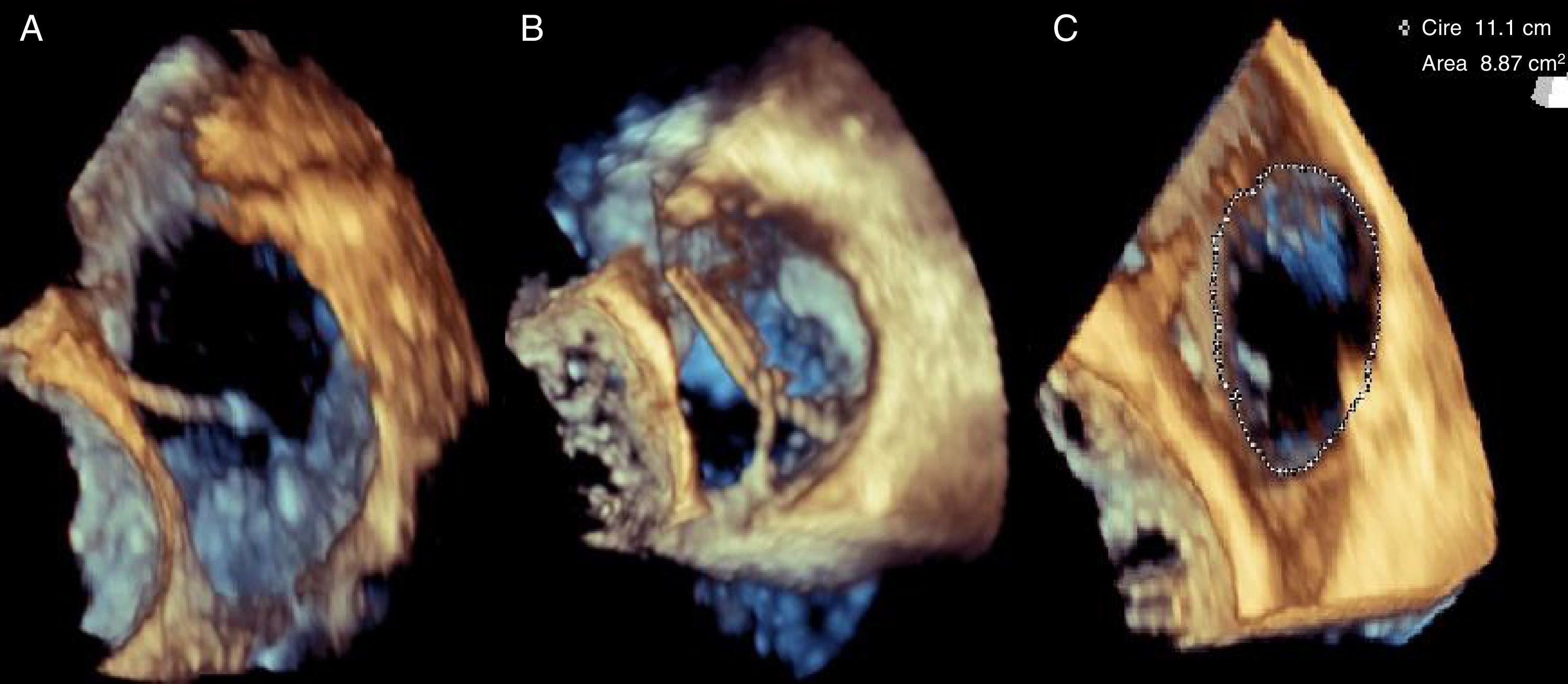
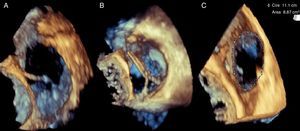
Summary descriptionThe technique used was similar to the one described by Schofer et al.14 In short, with this technique, the Mitralign system is used to place pledgeted sutures (via a trans-jugular approach) so that the tricuspid valve annulus can be plicated, thus leading to a bicuspidization of this valve.4,8,14 [Supplemental video 1 shows the different steps of the procedure, as assessed by transesophageal echocardiogram: A (pre-procedure, surgeon's view of the tricuspid valve), B–C (implantation of the first pledget), D (implantation of the second pledget), E–G (locking and bicuspidization of valve), H (post-procedure, surgeon's view of the tricuspid valve)]
Pre-procedure planning included transesophageal echocardiography (TEE) in order to assess tricuspid valve anatomy and physiology. The procedure per se was done with 2D and 3D TEE guidance, under general anesthesia, with anticoagulation by unfractionated heparin (under activated clotting time [ACT] guidance). Arterial access was obtained via a 6F right femoral cannula, and venous access was obtained via two 14F right jugular cannulas.
Case reportThe patient was a 77-year-old woman, who was referred to our department due to symptomatic heart failure despite diuretic therapy. She had undergone mitral valve replacement (with a mechanical valve prosthesis) ten years prior to referral. Other relevant pathological history included permanent atrial fibrillation and dyslipidemia.
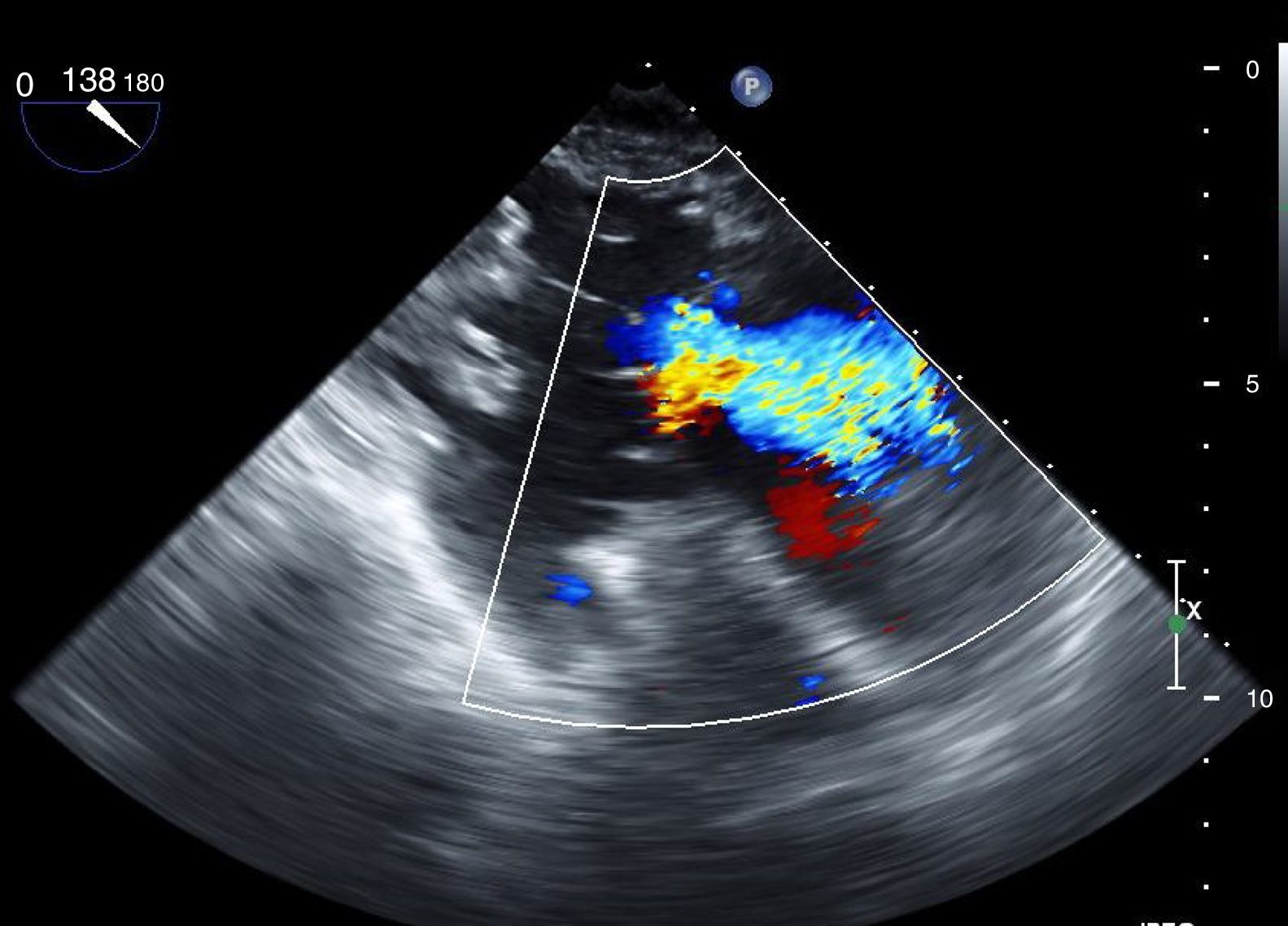
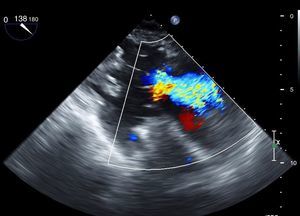
Her TEE showed biatrial dilatation, mild aortic regurgitation, a normally implanted and adequately functioning mitral valve prosthesis, moderate-to-severe TR and preserved biventricular function (Figure 1).
She had been assessed for possible surgical intervention, but due to perceived high surgical risk (namely in the context of previous cardiac intervention and overall clinical status, the patient presenting with a EuroSCORE [European System for Cardiac Operative Risk Evaluation] II score of 10.59% and a Log EuroSCORE of 29.30%), she was put forward for a percutaneous approach. After discussion and review of the case, she was accepted for percutaneous tricuspid valve intervention with the Mitralign system (compassionate use of the procedure).
Prior to implantation, her TEE showed a tricuspid annular area of 13 cm2 and an effective regurgitant orifice (ERO) area (calculated by the proximal isovelocity surface area [PISA] method) of 0.4 cm2.
The procedure was undertaken as previously described14 (supplemental video 1). A first pledget was placed in the tricuspid ring in the commissure between the septal and the posterior leaflet (Figure 2A); a second pledget was placed at about 24 mm in the valve annulus near the edge of the posterior leaflet. Subsequently, plication of the posterior leaflet was performed, with consequent bicuspidization of the valve, thus reducing the area of the valve ring to 9 cm2 (Figures 2B and 2C). No immediate complications arose.
After the procedure, the patient developed a femoral hematoma, which resolved with supportive care without the need for interventional treatment or blood transfusion. She had a favorable clinical course, and the remainder of hospitalization was uneventful, with the patient being discharged eight days after admission.
At the one-month follow-up, the patient maintained optimized pharmacological therapy, and was clinically improved (as self-reported), completing 280 meters during a six-minute walk test (versus 225 meters prior to intervention). Although clinically improved, diuretic utilization was maintained, and no down-grading of dose was performed at this follow-up.
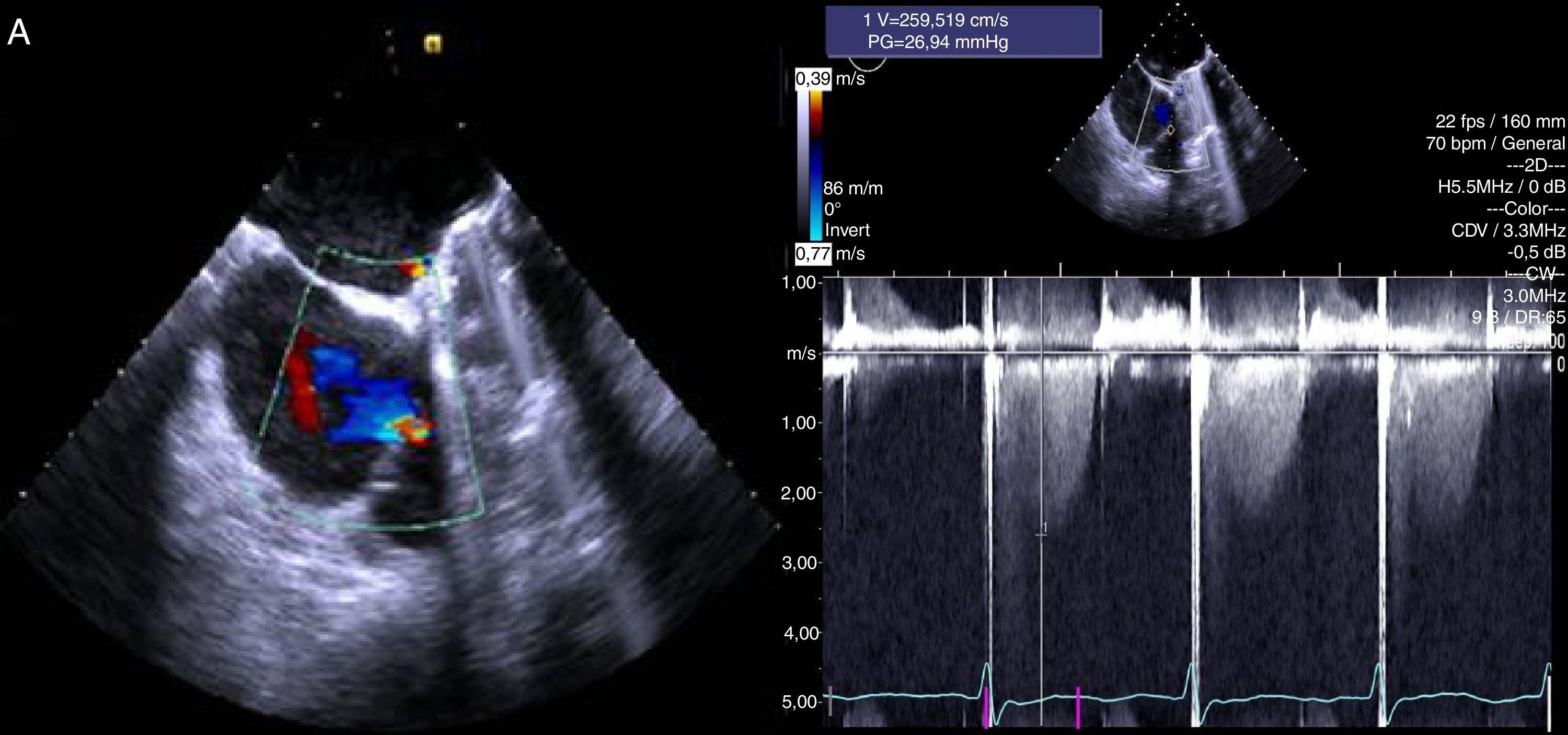
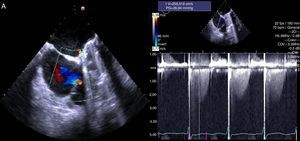
A follow-up TEE showed mild-to-moderate TR, with an ERO area (calculated by PISA) of 0.2 cm2 and a regurgitant volume of 18 mL (Figure 3), and preserved RV function.
DiscussionWe report the successful use of the Mitralign system in the treatment of a case of functional TR in a patient at high operatory risk (deemed not to be a candidate for surgical treatment), who was symptomatic despite diuretic therapy. Although she continued to require optimized pharmacological treatment, the patient's symptoms improved with a significant reduction in the degree of TR as assessed by TEE.
Functional TR occurring in patients after left-sided valve intervention presents important challenges, namely an increased surgical risk.3,16 Various factors, such as advanced age, frailty and different comorbidities add to this risk and, as such, there is still an unmet need in terms of the management of functional TR.17
Imaging techniques (with a special emphasis on echocardiography) are becoming increasingly crucial in the different stages of percutaneous procedures.18,19 In the case reported above, the use of echocardiography at different time points, and especially during the procedure (supplemental video 1; Figure 2), is critical for a good outcome. However, other modalities, such as cardiac computed tomography (which facilitates a precise assessment of the tricuspid annulus and surrounding structures, and also of possible access sites) are also gaining a prominent role in different percutaneous approaches.18,19 As different systems are being assessed in clinical practice, the interplay between imaging and intervention will become increasingly important.17–19
The limitations of our report include the fact that only one case, and with a limited follow-up (of only one month), was presented. As such, more data with a higher number of patients will be needed in order to further clarify the role of this procedure in routine clinical practice.20 The impact of this percutaneous tricuspid valve intervention in terms of morbidity (namely, if the symptomatic improvement will be maintained in mid- and long-term follow-up, and what the optimal pharmacological management will be after the intervention) and especially mortality, also need further clarification. Longer follow-up would also be important to see if a downgrade in diuretic therapy would be possible, while maintaining clinical improvement. In addition, the fact that this procedure is technically demanding (both in terms of the valve procedure per se, and the need for advanced imaging),8 is an important consideration. However, taking into account the scarcity of data concerning percutaneous TR intervention with this device,4,8,14 our results concur with those previously reported, and are promising given the clinical and echocardiographic improvement of the patient.
Although this is a new field, this description adds to our knowledge concerning percutaneous tricuspid valve intervention, a field whose complexity is only just beginning to be grasped.
Conflicts of interestThe authors have no conflicts of interest to declare.