The LMNA gene encodes a group of proteins that have an important structural and functional role in the cell nucleus. Mutations in this gene have been found in 6% of all forms of dilated cardiomyopathy and in up to 33% of those with conduction system disturbances.
Aims and MethodsUsing a case report as an example, we performed a review of the literature on the pathophysiological mechanisms, clinical manifestations, risk stratification and treatment options of cardiac involvement in laminopathies.
Case reportWe present the case of a 46-year-old man, whose ECG showed bizarre voltage criteria for left ventricular hypertrophy and first-degree atrioventricular block, a dilated left ventricle with mildly impaired global systolic function and non-sustained ventricular tachycardia on Holter monitoring, and with a family history of sudden death. Genetic testing identified an LMNA mutation. No ventricular arrhythmias were induced during electrophysiological study. The patient is under close clinical and echocardiographic monitoring and an event loop recorder has been implanted.
DiscussionPhenotypically, myocardial involvement in laminopathies is indistinguishable from other forms of idiopathic dilated cardiomyopathy. Ventricular arrhythmias are common, but the best method for sudden death risk stratification has yet to be established. The few studies that have been performed, with a very limited number of patients, show that factors associated with an unfavorable prognosis are ejection fraction <45%, non-sustained ventricular tachycardia, male gender and any form of atrioventricular block. Given the lack of evidence, indications for an implantable cardioverter-defibrillator for primary prevention in this context are the same as conventional indications for other forms of idiopathic dilated cardiomyopathy.
ConclusionsCardiac involvement as a consequence of LMNA mutations generally has a more aggressive natural history than other forms of non-ischemic dilated cardiomyopathy. A high index of suspicion and prompt referral for genetic testing are essential for appropriate therapeutic management.
O gene LMNA codifica proteínas que têm um papel estrutural e funcional importante a nível do núcleo celular. As suas mutações foram encontradas em 6% de todas as formas de miocardiopatia dilatada (MCD) e em 33% das formas que cursam com perturbações no sistema de condução.
Objetivos e métodosPartindo da descrição de um caso clínico, é feita uma revisão da evidência existente acerca dos mecanismos fisiopatológicos, manifestações, estratificação de risco e tratamento das laminopatias com atingimento cardíaco.
Caso clínicoÉ apresentado o caso clínico de um homem de 46 anos com critérios de voltagem bizarros para hipertrofia ventricular esquerda no ECG, dilatação e ligeira depressão da função sistólica ventricular esquerda e bloqueio auriculoventricular de 1.° grau, arritmias ventriculares não mantidas polimórficas em Holter e história de morte súbita familiar. O teste genético foi positivo para mutação no gene LMNA. Foi submetido a estudo eletrofisiológico no qual não se induziram arritmias ventriculares. O doente foi mantido sob vigilância clínica e ecocardiográfica e implantado detetor de eventos.
DiscussãoFenotipicamente, o atingimento miocárdico é indistinguível do das outras formas de MCD idiopática. As arritmias ventriculares são frequentes e a forma de melhor estratificar o risco de morte súbita está ainda por definir. Estão disponíveis resultados de poucos estudos e com um número muito limitado de doentes, sendo que os fatores de mau prognóstico identificados por estes foram: fração de ejeção < 45%, TV não mantidas, sexo masculino e presença de qualquer forma de bloqueio auriculoventricular. Dada a fraca evidência disponível, as indicações formais para implantação de CDI em prevenção primária neste contexto não são ainda diferentes das indicações convencionais noutras formas de MCD idiopática.
ConclusãoO atingimento cardíaco como consequência da mutação no gene LMNA apresenta uma história natural geralmente mais agressiva do que a maior parte das demais formas de MCD não isquémica. Um índice de suspeição elevado e o pedido atempado do teste genético são essenciais para a estratégia terapêutica.
The proteins lamin A and C polymerize to form the nuclear lamina, a meshwork of filaments on the nucleoplasmic side of the nuclear envelope, which separates the internal nuclear membrane from chromatin1 and is found in all differentiated cells of the organism. This mesh has a structural function, maintaining the shape and size of the nucleus. Nuclear lamins also play a role in gene regulation, DNA replication, RNA splicing, anchoring of other nucleoplasmic proteins, function and position of nuclear pores and heterochromatin organization.2,3
LMNA, the gene encoding lamin A/C, is located on chromosome 1 (locus 1q21.2-21.3).4 In 1999, an LMNA mutation was shown to cause autosomal dominant Emery-Dreifuss muscular dystrophy.5
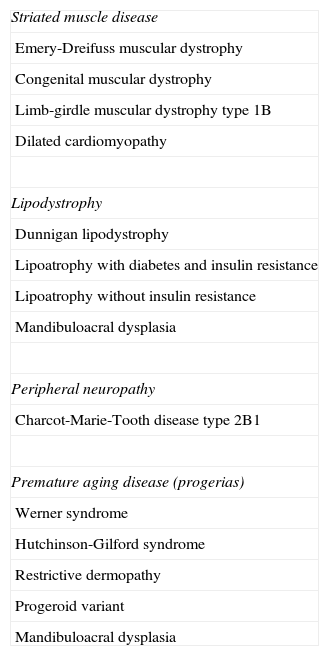
Since then, over 450 mutations in this gene have been described and are implicated in a range of other diseases, which differ in their phenotypic expression and affect various organ systems including muscles, fatty tissue and peripheral nerves, as well as systemic involvement in the case of progerias. These entities are termed laminopathies, as shown in Table 1.
Laminopathies.
| Striated muscle disease |
| Emery-Dreifuss muscular dystrophy |
| Congenital muscular dystrophy |
| Limb-girdle muscular dystrophy type 1B |
| Dilated cardiomyopathy |
| Lipodystrophy |
| Dunnigan lipodystrophy |
| Lipoatrophy with diabetes and insulin resistance |
| Lipoatrophy without insulin resistance |
| Mandibuloacral dysplasia |
| Peripheral neuropathy |
| Charcot-Marie-Tooth disease type 2B1 |
| Premature aging disease (progerias) |
| Werner syndrome |
| Hutchinson-Gilford syndrome |
| Restrictive dermopathy |
| Progeroid variant |
| Mandibuloacral dysplasia |
Many mutations linked to laminopathies also affect the heart, in the form of dilated cardiomyopathy (DCM), with or without involvement of other striated muscle, conduction disturbances and propensity for sudden death.
The mechanism through which lamin A/C deficiency causes these phenotypes is not fully understood. Two hypotheses have been proposed: one in which cell death is caused by loss of structural integrity at the nuclear level; and the other in which gene expression explains the phenotypic alterations through abnormal interaction with transcription factors in protein synthesis.2,6 The disease is expressed histologically by fibro-adipose degeneration and atrophy of the affected tissues. At the level of cell ultrastructure, there may be partial membrane rupture, disorganization of the nuclear membrane pores and vacuolization.7,8
From the standpoint of practical cardiological management, these diseases can be considered as a single entity – cardiomyopathy associated with LMNA mutations, with or without different types of muscle involvement.
The development and accessibility of genetic study has led to more frequent identification of LMNA mutations in patients who would previously have been diagnosed as having idiopathic DCM. One caveat is that, as has occurred in early studies of other diseases, the initial series reported and associated prognosis may have been biased by the natural tendency to identify only cases with a more marked phenotypic expression.
Case reportA 46-year-old man, a professional soccer player until the age of 34 and currently employed by a trucking company, was referred for cardiological assessment following detection of alterations on a routine ECG.
He denied having suffered chest pain, palpitations, syncope, fainting episodes, exertional or nocturnal dyspnea, or any muscular problems. There was no relevant personal medical history.
His family history included the death of a brother two years previously at age 60 following a fall from a motorcycle. According to his family, the autopsy report, to which we did not have access, revealed that trauma was not the cause of death but gave no further details.
Physical examination showed bradycardia (50 bpm) and deviation of the apical pulse to the left. No dysmorphism or muscle or joint malformations were observed and there were no changes on neurological examination.
The baseline ECG showed sinus bradycardia, first-degree atrioventricular block (AVB), with PQ interval of 240 ms, poor R-wave progression in the precordial leads and deep S waves (41 mV in V2). The resting echocardiogram revealed left ventricular dilatation with no wall thickening, mildly depressed ejection fraction (45%) and mild diffuse hypokinesia. The ultrasound findings were confirmed by cardiac magnetic resonance imaging, which also excluded areas of late enhancement, fatty infiltration and edema.
The patient underwent treadmill exercise echocardiography to investigate repolarization abnormalities suggestive of ischemia, arrhythmia and overall contractility. He achieved 14 min 48 s with the Bruce protocol. Increasingly frequent polymorphic ventricular extrasystoles were observed, with wide QRS complexes, and at peak exercise, pairs with the R wave close to the T peak. Ventricular contractility at peak exercise was strong, with almost complete systolic obliteration of the left ventricular cavity.
On 24-hour Holter monitoring, ventricular tachycardia (VT) with five bizarre polymorphic complexes were documented, together with a period of idioventricular rhythm at 70 bpm.
In the light of the findings of mild systolic dysfunction, first-degree AVB and sinus bradycardia, arrhythmic response to exercise and a short run of polymorphic VT, the patient was referred for genetic testing for LMNA mutations. The mutation c.1039G>A was found in heterozygosity in exon 6 of the lamin A/C gene, which leads to substitution of an amino acid at position 347 of the protein (p.Glu347Lys) and is a known cause of DCM.
It was decided to perform electrophysiological study (EPS) for stratification of arrhythmic risk, which showed an atrial-His interval of 186 ms, His-ventricle interval of 60 ms, and an antegrade Wenckebach point of 635 ms. Sinus node recovery time was normal. Right ventricular pacing in the apex and outflow tract with 600- and 400-ms drive cycle lengths and up to three extrastimuli at intervals of at least 200 ms did not trigger sustained ventricular arrhythmias.
Given the failure to induce ventricular arrhythmias during EPS and the patient's refusal to have an implantable cardioverter-defibrillator (ICD), it was decided to maintain clinical follow-up and six-monthly echocardiograms and to implant an event loop recorder with remote monitoring.
The results of genetic testing of the patient's first-degree relatives are awaited.
DiscussionNo specific feature has so far been identified that distinguishes cardiomyopathy associated with LMNA mutations from other forms of idiopathic DCM. It is characterized by dilatation and systolic dysfunction of one or both ventricles, myocyte destruction and myocardial fibrosis,9 and it is thus necessary to investigate more common etiologies of DCM.
LMNA mutations are found in 6% of all cases of DCM,10,11 in 7.5% of familial forms and in 3.6–11% of sporadic forms.12 They have also been identified in 33% of DCM patients with conduction system disease13; the prevalence of variants of uncertain significance in the general healthy population is estimated at 4%.14
In Portugal, the incidence of this etiology in patients with non-ischemic DCM is currently being assessed in the FATIMA study, mutations in the LMNA gene being investigated in all the subjects included.15
While the pattern of transmission is generally autosomal dominant, cases have been reported of an autosomal recessive pattern and of sporadic mutations. Penetrance is virtually 100% in carriers by the age of 60, with phenotypic expression of varying severity.16
The conduction system can be affected at practically all levels, and disturbances typically occur before ventricular dilatation.
Of the more than 30 genes in which mutations have been identified as causing DCM, only two are also associated with conduction disturbances: LMNA and SCN5A.12,17 Thus, the presence of DCM and conduction disorders should arouse a high level of suspicion, and an even higher level when there is also evidence of skeletal muscle abnormalities. Genetic testing for LMNA and SCN5A mutations in the presence of DCM of undetermined etiology and first-degree or higher AVB is a class I recommendation in the recent HRS/EHRA expert consensus statement.14
Tachyarrhythmias can also occur in the early phase of the disease, before and independently of the development of ventricular dilatation, sudden death being the first manifestation in some cases. In a study by van Berlo et al.,18 46% of mortality was due to sudden death, compared to 12% due to pump failure. Furthermore, 43% of the victims of sudden death had pacemakers for conduction system disease.
In a recent reference study,19 the incidence of sudden death, fatal or aborted after cardiopulmonary resuscitation or ICD shock, was 18% in a mean follow-up of 43 months. Mean age at death was 50±11 years. Independent predictors of sudden death were ejection fraction <45% at the beginning of follow-up, documented non-sustained VT and male gender. No patient with none of these risk factors suffered malignant ventricular arrhythmias, while these occurred in 1.7%, 27% and 54% of those with one, two or three risk factors, respectively. A recent study of 41 patients concluded that the best predictor of arrhythmic risk was the presence of first-degree AVB.20
The natural history of DCM due to LMNA mutations is aggressive. One epidemiological study estimated that 55% of carriers die from cardiovascular cause or are referred for transplantation by the age of 60, compared to only 11% of idiopathic DCM patients without mutations.12
Characteristically, arrhythmic manifestations begin in the third decade of life (over 90% of patients present at this age).18 Conduction disturbances warrant pacemaker implantation in 44% of patients, although this does not necessarily protect them from sudden death.18 In typical cases, signs of heart failure become apparent 15–20 years after the appearance of arrhythmias.
At present there is no specific treatment for cardiolaminopathies. However, the observation that the enzymes ERK 1/2 and JNK are overexpressed in carriers of LMNA mutations21 has opened up a line of research into the effect of pharmacological blockade of these pathways in mouse models,22 but this has yet to be tested in humans.
Drug therapy is in accordance with state-of-the-art treatment for other forms of DCM, but it is not clear whether use of the standard drugs to slow disease progression is warranted in silent carriers.
ICD implantation should be considered when arrhythmia or ventricular dilatation is documented in patients with mutations, especially when two or more of the above risk factors are present. This approach is of course not based on prospective clinical trials as it is a recently described rare disease, and thus has a level of evidence C. The incidence of sudden death in patients with pacemakers is such that some authors recommend ICD implantation for primary prevention in pacemaker candidates.23
There is as yet no evidence to support prophylactic ICD implantation in asymptomatic carriers. The role of EPS in stratifying risk for tachycardia and bradycardia has also yet to be established.
Some known risk factors were present in the case presented, including male gender, non-sustained VT on Holter monitoring, first-degree AVB and ventricular dilatation. Nevertheless, given the lack of indications for ICD implantation or pacemaker with a level of evidence A or B (no higher than first-degree and predominantly supra-Hisian AVB and asymptomatic) and the failure to induce ventricular arrhythmias on EPS (of uncertain significance), together with the patient's refusal of this option, it was decided to implant an event loop recorder for remote continuous heart rhythm monitoring to detect conduction blocks or ventricular arrhythmias, even if asymptomatic.
ConclusionMutations in the lamin A/C genes result in the phenotype of various diseases, most related to the musculoskeletal system. Cardiac involvement can be manifested by dilatation and systolic dysfunction, ventricular arrhythmias and conduction disturbances. Male gender, non-sustained VT on Holter monitoring, increased PR interval and ejection fraction <45% are the risk factors for sudden death so far described in small series. The role of EPS in stratifying arrhythmic risk has yet to be established.
A high index of suspicion and referral for genetic testing are essential to improve the prognosis of affected patients given the particularly aggressive course of the disease compared to most other forms of DCM.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Cabanelas N, Martins VP. Laminopatias: uma caixa de Pandora com insuficiência cardíaca, bradiarritmias e morte súbita. Rev Port Cardiol. 2015;34:139.