To study the differences between controlled and not controlled hypertensive patients.
MethodsThis was a cross-sectional observational study of the hypertensive population on the lists of three general practitioners in the district of Coimbra in central Portugal in 2013, with a margin of error of 6% and 95% confidence interval in each sample, organized in ascending order of health care user numbers. Data were gathered electronically by the investigators after approval by the Regional Health Authority's ethics committee.
ResultsA sample of 201 individuals was studied, of whom 104 (51.7%) were male and 86 (42.8%) were aged under 65 (p=0.127 for gender and age-group). Hypertension was controlled in 130 (64.7%). We found significant differences in target organ damage, more frequent in those with controlled hypertension (33.1% vs. 19.7%, p=0.031), in hypertension control, better in those taking at least one anti-hypertensive drug at night (56.9% vs. 29.6%, p=0.001), and in prescription of non-steroidal anti-inflammatory drugs, more frequent in those with uncontrolled hypertension (11.3% vs. 3.8%, p=0.043).
ConclusionHypertension control is significantly associated with target organ damage, taking at least one anti-hypertensive drug at night and not taking non-steroidal anti-inflammatory drugs simultaneously.
Determinar a prevalência e comparar diferenças entre pacientes hipertensos controlados e não controlados.
MetodologiaEstudo observacional, analítico, em junho de 2013, na população de três ficheiros clínicos de médicos de uma unidade de saúde familiar no concelho de Coimbra, com hipertensão arterial (HTA) diagnosticada e registada pela codificação ICPC-2 (com e sem complicações) até ao dia 13 de maio de 2013. Amostra calculada para um intervalo de confiança de 95% e margem de erro de 6% em cada um dos ficheiros, após obtenção de listagens por ordem ascendente do número nacional de utente, assumindo uma frequência de controlo de 50%. Colheita dos dados pelos autores, por consulta de todos os processos aleatorizados, com reposição, no programa específico de HTA e no ambiente de prescrição do serviço de apoio ao médico (SAM), após parecer positivo da Comissão de Ética da Administração de Saúde Regional do Centro. Controlo de HTA se nas três últimas espaçadas leituras o valor era inferior a 140/90 mmHg.
ResultadosEstudou-se uma amostra de n = 201 indivíduos, sendo 104 homens (51,7%) e tendo menos de 65 anos 86 (42,8%) (p = 0,127 entre sexo e grupo etário). Para n = 130 (64,7%) da amostra há controlo da HTA. A lesão em órgão-alvo é significativamente mais frequente nos pacientes com HTA controlada (33,1 versus 19,7%, p = 0,031). Quando há toma de pelo menos um medicamento à noite há maior frequência de controlo (56,9 versus 29,6%, p < 0,001). A simultaneidade de prescrição de anti-inflamatórios não esteroides é mais frequente nos pacientes com HTA não controlada (11,3 versus 3,8%, p = 0,043).
ConclusãoSão fatores significativamente mais frequentes no controlo da HTA o prévio acidente cardiovascular, a toma de pelo menos um anti-hipertensor à noite e a ausência de simultânea prescrição de anti-inflamatórios não esteroides.
Hypertension (HTN) is a common disease with a wide range of causes, high morbidity and mortality and considerable drug therapy costs, and is the subject of three sets of guidelines by the Portuguese Directorate-General of Health.1–3 The prevalence of HTN in Portugal is estimated at 42.62%. According to the VALSIM study, 47.62% of hypertensive patients are prescribed a single anti-hypertensive drug, 36.16% two drugs and 16.22% three or more drugs; diuretics are prescribed in 47.40%.4
Various studies2,5–8 support initial treatment with diuretics, and bedtime chronotherapy, in which at least one drug is taken at night, has been shown to reduce cardiovascular events due to HTN in the long term.9
The prevalence of HTN increases with age.4,7 It is also known that some medications, particularly non-steroidal anti-inflammatory drugs (NSAIDs), result in a lower level of HTN control.9
Hypertensive therapy should include at least two different classes of drugs, and chlorthalidone should be the first-line agent, despite minor clinical issues and changes in laboratory parameters associated with this drug.2,7,8
Differences in patients’ individual circumstances can lead to different attitudes to adherence to therapy, particularly a previous vascular event, associated disease or risk factors. What is undeniable is that in Portugal, few treated hypertensive patients are in fact controlled.11–13
Adherence to therapy is essential in HTN control and non-adherence should be viewed not as forgetfulness, but rather as the result of the patient's subjective experience of living with HTN and the ability to accept the diagnosis and its treatment, since it usually does not give rise to symptoms or signs until complications appear. Cardiovascular events or complications may thus be related to non-adherence to therapy.12
The need to treat must be balanced against the risk of harm or waste, particularly in cases of moderate HTN, as shown in a 2012 review.14 There is debate concerning which cut-offs should be used to define HTN – the current 140/90 mmHg or the previous 160/100 mmHg – in order to determine whether the investment in anti-hypertensive therapy on the part of individuals, their families and society is justified.15,16 There may be other factors, including diet, medications and level of awareness, that physicians should take into consideration to improve the efficiency of HTN treatment.17
This situation highlights the need to understand the differences between patients with controlled and uncontrolled HTN.
ObjectiveOur aim was to study the differences between the characteristics of patients with controlled and uncontrolled HTN, particularly in terms of age, gender, previous cardiovascular events, comorbidities, number and type of anti-hypertensive drugs prescribed, medication with chlorthalidone, taking at least one anti-hypertensive drug at night, and concomitant use of NSAIDs.
MethodsThis was a cross-sectional observational study, using random sampling with replacement, of the hypertensive population of three general practitioner lists in a family health unit in the municipality of Coimbra in June 2013, with an International Classification of Primary Care second edition (ICPC-2) classification of HTN (with or without complications) up to May 13, 2013, the date on which the case lists to be studied were drawn up. The sample size was calculated for a margin of error of 6% and 95% confidence interval for each list, with a control frequency of 50%. The lists were organized in ascending order of health care user numbers, and the data were gathered electronically by the investigators from all the records of hypertensive patients selected by random sampling from the lists registered in the Medical Support Service database (SAM), together with prescription data. If no data were available on blood pressure (BP) measurement in the previous nine months, the patient immediately before on the list was selected. If data were unavailable in this case also, the patient immediately after on the list was selected. In the continued absence of data, the previously defined randomization process was followed, in other words, the fifth patient on the list after the original patient was selected. Agreement was obtained from the general practitioners involved, as well as approval from the Regional Health Authority's ethics committee.
BP values were taken as the mean of the last three measurements registered in the SAM database, over a minimum period of nine months, three readings being taken at each consultation. Medication was recorded by International Common Denominations. Anti-hypertensive medication taken at night was determined by searching the electronic prescriptions for each patient over the previous nine months, as was simultaneous prescription of NSAIDs, a positive association being assumed when there was continuous prescription of NSAIDs in the previous nine months.
The study was based on the chronic disease classifications recorded by the physician as the patient's personal history in their medical record in accordance with standard definitions. The following terms are used in the HTN program of SAM:
- •
Target organ damage: stroke/transient ischemic attack, congestive heart failure, left ventricular hypertrophy, renal disease, atheromatosis, retinopathy;
- •
Associated disease: nephropathy, coronary artery disease, vascular disease, myocardial infarction;
- •
Other disease: diabetes, glomerular disease, dyslipidemia.
The diagnoses of the diseases in each of the above sections are those universally accepted on the basis of laboratory tests and diagnostic exams, and are entered into the database by the attending physician.
Dichotomous variables were analyzed on the basis of their presence or absence and the study population was divided into two age-groups: age ≥65 and age ≤64 years.
A descriptive and parametric inferential statistical analysis was performed after normal distribution of data was confirmed. The Student's t test was used for unpaired variables, and the chi-square test was used to compare nominal variables.
ResultsOf a total population of 972 (HTN prevalence 20.2%), a sample of 201 individuals was studied, of whom 104 were male (51.7%), and 86 (42.8%) were aged under 65 (p=0.127 for gender and age-group).
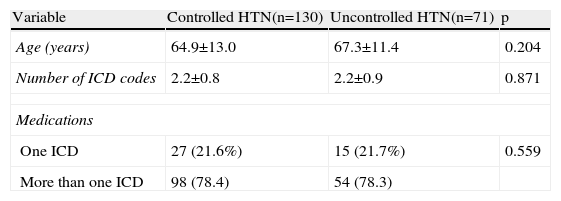
HTN was controlled in 64.7% (n=130) of the sample (Table 1). Target organ damage was significantly more frequent in those with controlled HTN (33.1% vs. 19.7%, p=0.031), as was taking at least one anti-hypertensive drug at night (56.9% vs. 29.6%, p<0.001), while simultaneous use of NSAIDs was more frequent in those with uncontrolled HTN (11.3% vs. 3.8%, p=0.043).
Characteristics of patients with controlled and uncontrolled hypertension.
| Variable | Controlled HTN(n=130) | Uncontrolled HTN(n=71) | p |
| Age (years) | 64.9±13.0 | 67.3±11.4 | 0.204 |
| Number of ICD codes | 2.2±0.8 | 2.2±0.9 | 0.871 |
| Medications | |||
| One ICD | 27 (21.6%) | 15 (21.7%) | 0.559 |
| More than one ICD | 98 (78.4) | 54 (78.3) | |
| n (%) | n (%) | ||
| Gender | |||
| Male | 64 (49.2) | 34 (56.3) | 0.207 |
| Female | 66 (50.8) | 31 (43.7) | |
| Age-group | |||
| ≤64 years | 58 (44.6) | 28 (38.4) | 0.288 |
| ≥65 years | 72 (55.4) | 43 (60.6) | |
| Target organ damage | |||
| Yes | 43 (33.1) | 14 (19.7) | 0.031 |
| No | 87 (66.9) | 57 (80.3) | |
| Associated disease | |||
| Yes | 26 (20.0) | 16 (22.5) | 0.401 |
| No | 104 (80.09 | 55 (77.5) | |
| Other disease | |||
| Yes | 97 (74.6) | 47 (66.2) | 0.136 |
| No | 33 (25.4) | 24 (33.8) | |
| Diuretics | |||
| Yes | 81 (64.8) | 48 (69.6) | 0.305 |
| No | 44 (35.2) | 21 (30.4) | |
| Chlorthalidone | |||
| Yes | 22 (16.9) | 9 (12.7) | 0.280 |
| No | 108 (83.1) | 62 (87.3) | |
| Prescription of at least one anti-hypertensive drug at night | |||
| Yes | 74 (56.9) | 21 (29.6) | <0.001 |
| No | 56 (43.1) | 50 (70.4) | |
| Simultaneous use of NSAIDs | |||
| Yes | 5 (3.8) | 8 (11.3) | 0.043 |
| No | 125 (96.2) | 63 (88.7) | |
HTN: hypertension; ICD: International Common Denomination; NSAIDs: non-steroidal anti-inflammatory drugs.
The results showed that 66.5% of hypertensives were medicated with diuretics, and of these, 24.3% (n=31) were taking chlorthalidone; there was a low rate of prescription of NSAIDs (6.5%, n=13). Eighty-six patients (42.8%) were taking two drugs, and 57 (28.4%) were taking three.
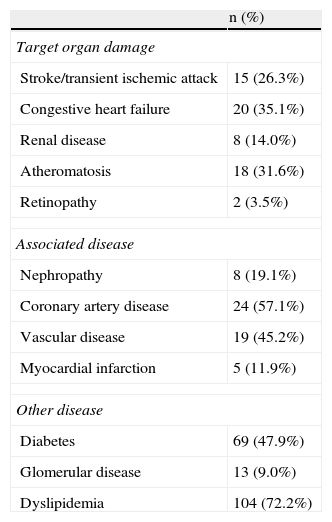
Target organ damage was recorded in 28.4% of the sample, associated disease in 29.9% and other disease in 28.4%, as shown in Table 2.
Disease history according to the records of the Medical Support Service database.
| n (%) | |
| Target organ damage | |
| Stroke/transient ischemic attack | 15 (26.3%) |
| Congestive heart failure | 20 (35.1%) |
| Renal disease | 8 (14.0%) |
| Atheromatosis | 18 (31.6%) |
| Retinopathy | 2 (3.5%) |
| Associated disease | |
| Nephropathy | 8 (19.1%) |
| Coronary artery disease | 24 (57.1%) |
| Vascular disease | 19 (45.2%) |
| Myocardial infarction | 5 (11.9%) |
| Other disease | |
| Diabetes | 69 (47.9%) |
| Glomerular disease | 13 (9.0%) |
| Dyslipidemia | 104 (72.2%) |
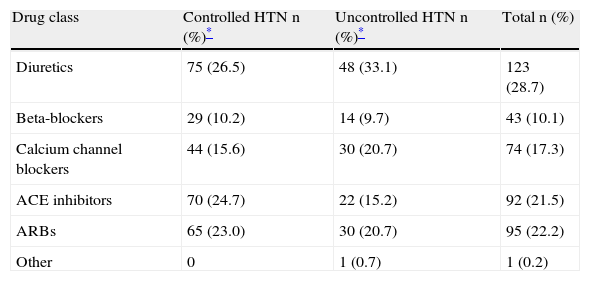
Table 3 shows the distribution of the various drug classes among 194 treated hypertensives in terms of controlled or uncontrolled HTN, which reveals significant differences.
Distribution of the various drug classes prescribed in patients with controlled and uncontrolled hypertension.
| Drug class | Controlled HTN n (%)* | Uncontrolled HTN n (%)* | Total n (%) |
| Diuretics | 75 (26.5) | 48 (33.1) | 123 (28.7) |
| Beta-blockers | 29 (10.2) | 14 (9.7) | 43 (10.1) |
| Calcium channel blockers | 44 (15.6) | 30 (20.7) | 74 (17.3) |
| ACE inhibitors | 70 (24.7) | 22 (15.2) | 92 (21.5) |
| ARBs | 65 (23.0) | 30 (20.7) | 95 (22.2) |
| Other | 0 | 1 (0.7) | 1 (0.2) |
Diuretics were the most commonly prescribed drug class, followed by angiotensin type 1 receptor blockers. Diuretics were more frequently used in those with uncontrolled HTN, while drugs that act on the renin–angiotensin–aldosterone system were more frequent in those with controlled HTN. The drug class most commonly prescribed as monotherapy was angiotensin-converting enzyme inhibitors (n=17, 8.5%).
DiscussionIt is important to know the determinants of good treatment outcomes that can be assessed by measurable data, particularly when considerable financial resources are involved, both structural and procedural, as well as costs that represent a heavy burden for individuals, families and society.
Various types of study can be used for this purpose. We opted for a cross-sectional, population-based study, assessing a random sample of hypertensives so as to reduce bias. The sample size was considered sufficient to demonstrate the results.
In a study that included 86 patients (42.8%) aged over 65, we used a cut-off of 140 mmHg and 90 mmHg for systolic and diastolic BP, respectively, to define hypertension, although different cut-offs have been proposed.1,15,16
According to the national and international literature, the prevalence of controlled HTN remains low in Portugal, although this was not the case in our study, 64.7% of hypertensives being controlled, better than previous studies, which reported 11.2% in 2011 and 42.6% in 2012.10,11
There was also a non-significant tendency for men to show a lesser degree of HTN control, a finding that should prompt greater therapeutic and educational efforts in those treating them.12
The fact of having suffered a vascular event is an important factor in control; it appears that patients who have suffered an event are more careful of their own health or are more closely monitored by those treating them, a factor that deserves study. Greater efforts are required by physicians and other health professionals in terms of therapeutic and educational intervention in this health problem, to raise awareness among patients and improve their ability to accept the diagnosis and its treatment.12,13
Our results conflict with those reported in another population-based study in Greater Porto, but this focused mainly on patient awareness of HTN.14
Patients with uncontrolled HTN showed a non-significant tendency for a higher prevalence of associated disease and less frequent use of chlorthalidone. Increased use of this thiazide diuretic may produce better results, confirming the findings of the ALLHAT trial.2,8
Prescription patterns were similar to those described in other studies in Portugal, with high levels of prescription of drugs acting on the renin–angiotensin–aldosterone system, which may bring considerable future benefits through better control of central arterial pressure.18–21 However, our study found a higher proportion of patients medicated with two or more drugs, which may explain the better treatment performance, as reflected in the percentage of patients with controlled HTN.18,19 Taking at least one anti-hypertensive drug at night has a significant impact on BP control, which corroborates the findings of the MAPEC study,9 and indicates that bedtime chronotherapy should be implemented.
There was a low prevalence of simultaneous prescription of NSAIDs in this population, possibly the result of studies carried out with prescribing doctors.22
Our study assessed the practical outcomes of the interaction between patient, care team, and medication through analysis of computerized records. Other factors were not studied, such as adherence to therapy and enablement instruments employed during consultations, and whether these diminish over time, which can have a marked effect on HTN control and should be addressed in future studies.23–28
ConclusionIn this population-based study of a random and representative sample, hypertensive patients who had previously suffered a cardiovascular event were better controlled. There was a significant association between taking at least one anti-hypertensive drug at night, as well as the absence of simultaneous prescription of NSAIDs, and better HTN control. Albeit without statistical significance, the study also found that younger patients showed no better control, associated disease did not result in worse control, a greater number of anti-hypertensive drugs improves control, diuretics do not improve control and use of chlorthalidone is associated with better HTN control. In the last three office BP measurements, 64.7% of the patients in our sample had their HTN controlled.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Santiago LM, Pereira C, Botas P, Simões AR, Carvalho R, Pimenta G, et al. Pacientes com hipertensão arterial em ambiente de medicina geral e familiar: análise comparativa entre controlados e não controlados. Rev Port Cardiol. 2014;33:419–424.