Factor VIII is a clotting factor that plays a crucial role in the coagulation cascade. Above-normal levels are found in 11% of the general adult population. Various studies have established a causal association between elevated factor VIII and venous thrombosis; some studies also suggest a relation with arterial thrombosis, particularly myocardial infarction and stroke.
We report the case of a 36-year-old man with obesity, smoking and dyslipidemia as cardiovascular risk factors and a history of acute myocardial infarction at age 26. He was admitted to the coronary care unit with a diagnosis of ST-elevation myocardial infarction. Coronary angiography showed a thrombus in the distal segment of the first obtuse marginal artery, which was causing the obstruction. The thrombus was aspirated but there was no reflow. A coagulation study revealed elevated factor VIII; other parameters were normal.
Even though this patient presented several cardiovascular risk factors, we highlight the need for more studies on the effect of elevated factor VIII on thrombus formation leading to acute coronary syndrome. Another important question is the use of oral anticoagulation in these patients as an integral part of the management of acute coronary syndrome.
O fator VIII é um cofator procoagulante, que desempenha um papel crucial na cascata da coagulação intrínseca. Níveis elevados podem ser encontrados em cerca de 11% da população geral adulta. Vários estudos têm evidenciado, de forma consistente, que o seu aumento parece ser um fator de risco para tromboembolismo venoso; alguns estudos relatam também uma provável associação com a trombose arterial, nomeadamente a doença arterial coronária e o acidente vascular cerebral.
Os autores apresentam um caso de um doente do género masculino, de 36 anos, com fatores de risco cardiovascular conhecidos, nomeadamente obesidade, tabagismo e dislipidemia mista e com antecedentes pessoais de enfarte agudo do miocárdio aos 26 anos. Internado num serviço de cardiologia por enfarte agudo do miocárdio com supradesnivelamento do segmento ST. A coronariografia evidenciou a presença de trombo oclusivo no segmento distal da artéria obtusa marginal, o qual foi aspirado, tendo-se verificado posteriormente a ocorrência de no reflow. O estudo analítico realizado posteriormente revelou uma elevação dos níveis de fator VIII; sem outras alterações no estudo de trombofilias.
No caso clínico descrito embora o doente apresente vários fatores de risco cardiovascular realça-se a necessidade de se efetuarem mais estudos sobre o papel do fator VIII na formação de trombo responsável por síndroma coronária aguda e sobre a necessidade de efetuar o seu doseamento perante a evidência de trombo formado. Outra questão pertinente que se levanta é o papel da anticoagulação nestes doentes como parte integrante da terapêutica em contexto de síndroma coronária aguda.
The balance between fibrin formation and fibrinolysis can be disturbed by reduced blood flow, changes in the vascular wall and hypercoagulability, all of which can favor fibrin formation and may lead to the formation of occlusive thrombi.1
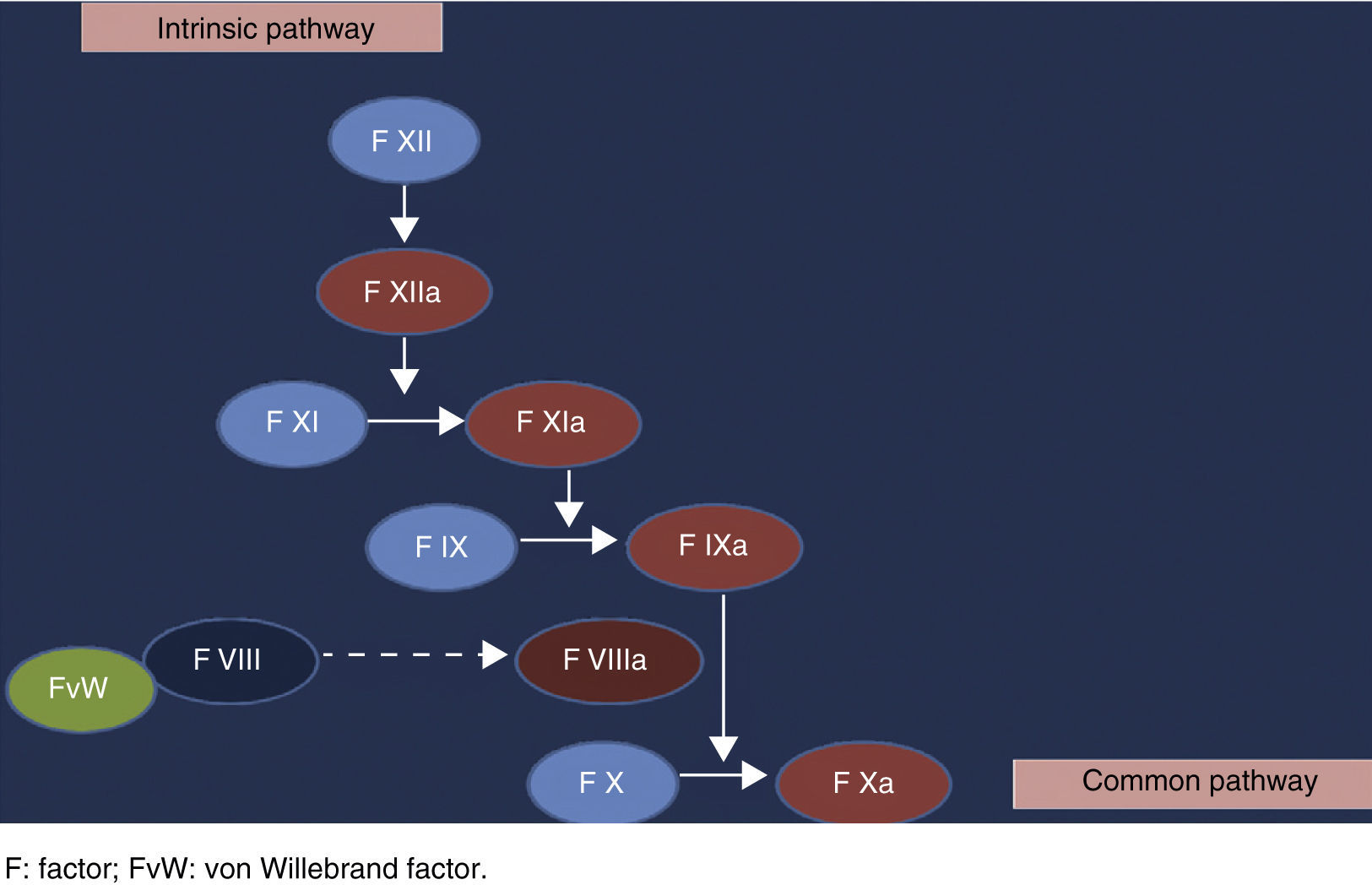
Factor VIII is a clotting factor that plays a crucial role in the coagulation cascade.2 It forms a complex with von Willebrand factor, which protects it from proteolysis and concentrates it at the site of hemostasis. Once activated, factor VIII separates from von Willebrand factor and the resulting factor VIIIa binds to factor IXa, forming an enzyme complex on the membrane surface that converts factor X into factor Xa3 (Figure 1).
Various studies in recent years have established a causal association between elevated factor VIII levels and venous thrombosis.1,2,4–8 Although further studies are needed, some authors also suggest an increased risk for arterial thrombosis, particularly myocardial infarction (MI) and stroke.1,5,9–12
Case reportThe authors present the case of a 36-year-old man, with obesity (body mass index 30.5 kg/m2), smoking and mixed dyslipidemia as cardiovascular risk factors; he had a history of MI at age 26, when coronary angiography identified a lesion in the right posterolateral branch, which was treated by balloon angioplasty (without stenting).
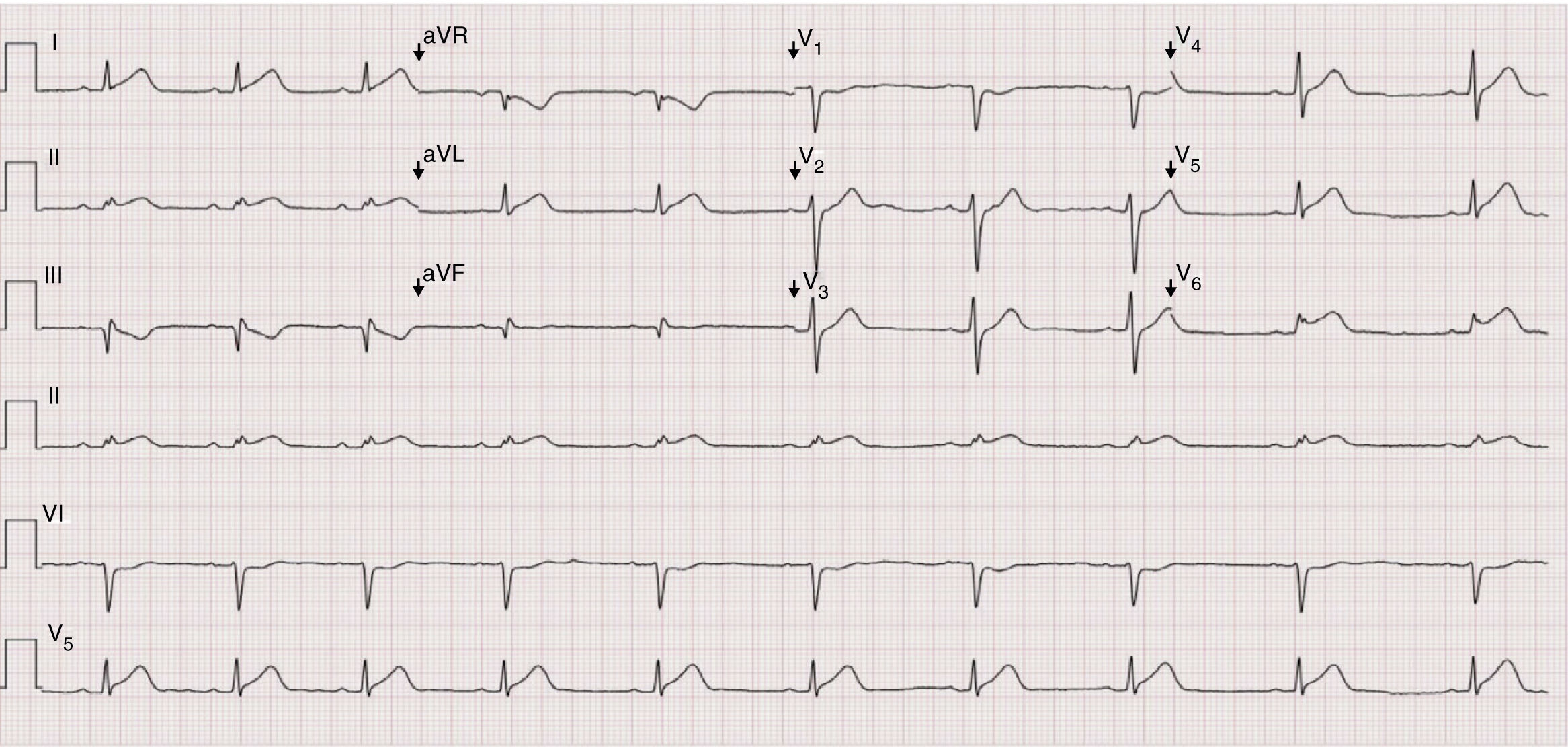
He came to the emergency department due to sudden-onset intense chest pain that had begun two hours earlier after lunch; complete symptom relief was achieved following administration of antiplatelets, nitrates and morphine. On physical examination he was hemodynamically stable, with no relevant alterations. The 12-lead electrocardiogram showed sinus rhythm, heart rate 60 bpm, poor R-wave progression, ST-segment elevation in V5, V6, DI, DII and aVL, and q waves in DIII (Figure 2). Laboratory tests revealed hemoglobin 16.3 g/dl, white cell count 10100×106/l, platelets 207000×106/l, creatinine 0.9 mg/dl, urea 35.2 mg/dl, and normal ionogram; initial troponin I was 0.04 ng/ml, subsequently rising to >50 ng/ml. Transthoracic echocardiography showed good global systolic ventricular function, with no wall motion abnormalities or other alterations.
The patient was admitted to the coronary care unit with a diagnosis of ST-elevation MI. Coronary angiography showed a thrombus in the distal segment of the first obtuse marginal artery, which was causing the obstruction. The thrombus was aspirated but there was no reflow; no stent was placed. The previously treated lesion in the right posterolateral branch showed no evidence of restenosis (Figure 3).
The patient remained asymptomatic during hospital stay. Further laboratory tests showed normal thyroid function, mixed dyslipidemia (total cholesterol 264 mg/dl, HDL cholesterol 41 mg/dl, LDL cholesterol 180 mg/dl, and triglycerides 214 mg/dl), and homocysteine within the normal range (13 μmol/l); thrombophilia testing detected elevated factor VIII (236%) only.
Discussion and ConclusionsElevated factor VIII (>150 IU/dl) is found in 11% of the general adult population.6 There has been much debate over the years as to whether factor VIII is a thrombotic agent or merely a marker of inflammation. Although factor VIII may be increased in situations that induce an acute phase response, including MI, surgery and sepsis, according to some authors its association with venous and arterial thrombosis not only reflects a prothrombotic inflammatory process but is a direct causal mechanism in thrombosis and therefore a therapeutic target.13 This thrombogenic effect has a non-linear relationship with elevations in factor VIII levels,2 and appears to depend on the extent of vascular injury.13
Regulation of plasma factor VIII levels is complex and involves both genetic and acquired factors. Levels are higher in women, blacks, and individuals with blood groups other than O, high body mass index, diabetes or hypertriglyceridemia, as well as in other clinical situations including pregnancy, surgery, chronic inflammation, cancer, liver disease, hyperthyroidism, intravascular hemolysis and kidney disease. In many of these conditions, there is a concomitant increase in factor VIII and von Willebrand factor.1 Thus, one problem in clinical practice is the timing of factor VIII measurement, since levels may be elevated in acute phase responses and may not return to baseline levels for several months.1
Factor VIII is most commonly measured as factor VIII:C through changes in activated partial thromboplastin time, which is simpler but generates a larger number of false positives, due to activation of the coagulation cascade during blood collection or storage. An alternative technique is to measure factor VIII:Ag by ELISA, which is time-consuming but is not susceptible to coagulation cascade activation.1 Oral anticoagulation with warfarin does not appear to affect measurement of factor VIII levels.6,8
The case presented highlights the possible role of factor VIII in the etiology of arterial thrombosis, particularly in acute coronary syndromes. Others cases have been reported of acute coronary syndrome associated with elevated factor VIII in patients with no other known cardiovascular risk factors or significant underlying atheromatous disease.9,11 Although our patient had other cardiovascular risk factors, the question remains as to the contribution of factor VIII to the arterial thrombotic event, particularly in the absence of other documented angiographic lesions. The reliability of a single measurement is also questionable, since various other factors in this case, including the patient's acute coronary event, high body mass index and hypertriglyceridemia, could have affected the result; however, his factor VIII level was considerably higher than the reference value. The measurement should be repeated some time after the acute event and in the absence of other complications, in order to obtain the baseline value.
The link between factor VIII and venous thromboembolism is well documented, but an important question is whether patients with venous thrombosis should be screened for elevated factor VIII, since this increases the risk of both a first thrombotic event and of recurrent events,1,14 which suggests that prolonged anticoagulation may be necessary in these patients.6 The risk of recurrence approaches 30% two years after discontinuation of anticoagulation,7 but it has yet to be established how long an individual with elevated factor VIII should continue anticoagulant therapy.7
The diagnostic and therapeutic approach to arterial thrombosis is even less clear, particularly concerning the need to measure factor VIII in patients who have suffered an arterial thrombotic event and the initiation and duration of anticoagulant therapy when levels are elevated. There are cases in the literature of patients with acute coronary syndrome and elevated factor VIII but no other known cardiovascular risk factors who were prescribed anticoagulant therapy for six months.11
Thrombophilia testing is even more important in younger age-groups. Five to ten percent of infarctions occur in patients aged under 45, many of whom have none of the usual atherothrombotic risk factors.12 Thrombotic events in these patients that cannot be explained by conventional mechanisms should prompt investigation of thrombophilia, which should include factor VIII in the light of recent evidence.
It is also important to remember that relatives of patients with thrombophilic disorders may need counseling and risk assessment. More studies are required to determine whether screening relatives of patients with elevated factor VIII levels who have suffered a thrombotic event is justified.5
The aim of this article is thus to alert the medical community to a possible risk factor for acute coronary syndrome that has been the subject of an increasing number of studies over the years but that still requires further investigation. Elevated factor VIII may indeed be the cause of a significant number of cases of idiopathic hypercoagulability states and a contributing factor in thrombosis.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in the study.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Costa C, Alves M, Durão D, et al. Excesso de fator VIII em doente com síndroma coronária aguda. Rev Port Cardiol. 2014;33:181.e1–181.e4.