Heart failure is a common problem and a major cause of mortality, morbidity and impaired quality of life. Anemia is a frequent comorbidity in heart failure and further worsens prognosis and disability. Regardless of anemia status, iron deficiency is a common and usually unidentified problem in patients with heart failure. This article reviews the mechanisms, impact on outcomes and treatment of anemia and iron deficiency in patients with heart failure.
A insuficiência cardíaca é uma patologia comum e uma causa importante de mortalidade, morbilidade e deterioração da qualidade de vida. A anemia é uma comorbilidade frequente na insuficiência cardíaca e agrava o seu prognóstico e capacidade funcional. Independentemente da presença ou não de anemia, a deficiência de ferro é um problema associado à insuficiência cardíaca muitas vezes não identificado. Este artigo revê os mecanismos, impacto prognóstico e tratamento da anemia e deficiência de ferro.
A 72‐year‐old woman with a history of poorly controlled hypertension under diuretic therapy for the previous 10 years was assessed for fatigue and dyspnea on minimal exertion (NYHA class III). Her blood pressure was 150/85 mmHg and her heart rate was 88 bpm; she had faint crackles in the lung bases and ankle edema. The ECG showed voltage criteria for left ventricular hypertrophy. Her hemoglobin (Hb) level was 11.0 g/dl and her mean corpuscular volume was 85 fl, blood glucose 102 mg/dl, total cholesterol 190 mg/dl and creatinine 1 mg/dl. She was medicated with furosemide, a renin‐angiotensin system inhibitor and a beta‐blocker, and was referred for echocardiographic assessment.
What role did the patient's Hb of 11 g/dl play in her clinical setting?
IntroductionThe prevalence of heart failure (HF) is 1–2%, but may exceed 10% in individuals aged over 70.1,2 In Portugal, the prevalences of HF with systolic dysfunction and HF with preserved systolic function have been estimated at 1.3% and 1.7%, respectively, in a primary health care context.3
HF is associated with a marked decline in quality of life and high morbidity and mortality.4 Although treatment with renin‐angiotensin‐aldosterone system inhibitors and beta‐blockers can be effective, one‐year mortality is up to 20% and rehospitalizations for HF can reach 30%.5 However, the clinical course of HF is variable, due to the interaction of diverse demographic and clinical characteristics that affect prognosis, among them anemia and iron deficiency.6–8
Anemia in heart failureAnemia is a frequent comorbidity in HF. Its prevalence ranges between 4% and 55% depending on the study population and the cutoff values of Hb defined as the lower limit of normal.9 In a large cohort study published in 2003 of 12 065 patients with new‐onset HF in 138 centers in the Canadian state of Alberta, the prevalence was 17%.10 It is more common in women, the elderly and individuals with renal failure.
Anemia is associated with increased morbidity and mortality, as well as significant reductions in functional capacity, which is already impaired by HF.6–8,11,12 In the largest observational registry published, anemia was an independent indicator of prognosis after correction for numerous confounding factors.12
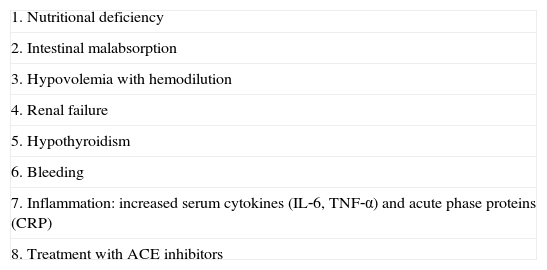
There are various causes of anemia in association with HF (Table 1), including renal failure and hypothyroidism, and occasionally low levels of vitamin B12 and folic acid.13 Another factor may be hemodilution, which can cause anemia due to expansion of plasma volume without any effective reduction in red blood cells. Angiotensin‐converting enzyme inhibitors, which are commonly used in HF treatment, can be associated with low Hb, probably by suppression of erythropoietin, while inflammatory cytokines such as interleukin‐1 and ‐6 and tumor necrosis factor alpha, which are elevated in severe HF, can reduce production of erythropoietin or increase resistance to its action. Finally, antiplatelet or anticoagulant therapy can cause gastrointestinal bleeding.14
Factors associated with anemia in patients with heart failure.
| 1. Nutritional deficiency |
| 2. Intestinal malabsorption |
| 3. Hypovolemia with hemodilution |
| 4. Renal failure |
| 5. Hypothyroidism |
| 6. Bleeding |
| 7. Inflammation: increased serum cytokines (IL‐6, TNF‐α) and acute phase proteins (CRP) |
| 8. Treatment with ACE inhibitors |
ACE: angiotensin‐converting enzyme; CRP: C‐reactive protein; IL‐6: interleukin‐6; TNF‐α: tumor necrosis factor alpha.
Although all of the above factors can play a part, iron deficiency anemia (IDA) is the most common form in HF.
IDA associated with HF may be absolute or functional. The following mechanisms are presumed to be involved in the development of absolute IDA, in which iron stores are depleted as indicated by serum ferritin <30 μg/l15: (i) insufficient dietary iron supply, (ii) intestinal malabsorption, impaired duodenal iron transport, drug interactions (e.g. omeprazole), or food reducing absorption, and (iii) gastrointestinal bleeding.
In a 2006 study of the causes of anemia in HF patients, de Silva et al. found low iron or ferritin levels in 43% of patients but microcytosis in only 6%.16 However, Nanas et al. detected iron deficiency in bone marrow in their study population, despite normal serum iron, ferritin and erythropoietin.17 This may be explained by diversion of iron from the marrow to storage sites of the reticuloendothelial system, where it is unavailable for erythropoiesis despite normal or high iron and ferritin levels, as seen in chronic disease.18
An important factor is transferrin saturation (TSAT). Normal TSAT ranges between 20% and 50%; values below 20% are seen in IDA and inflammation anemia. In a study of 157 patients with chronic HF, TSAT <20% was associated with higher NYHA functional class, lower peak oxygen consumption and greater mortality in two‐year follow‐up.19
Functional IDA is defined as insufficient iron supply to meet demands, despite abundant iron stores, because iron is locked within cells of the reticuloendothelial system and is unavailable for cell metabolism. One mechanism in functional IDA appears to be related to hepcidin, a protein that is central to regulation of iron metabolism. Hepcidin levels are elevated in the initial stages of HF but fall as the disease progresses; low levels are an independent marker of worse prognosis.15 Hepcidin binds to ferroportin, the only protein able to export intracellular iron, which is thereby degraded, preventing iron from re‐entering cells.15 This reduces iron absorption in the duodenum and causes iron to be retained in the reticuloendothelial system, reducing its concentration and availability in target tissues. Hepcidin also plays a part in erythropoiesis and in the innate immune response to pathogens.
Iron is essential for normal hematopoiesis; most of it is taken up by erythroblasts and reticulocytes for Hb synthesis. Iron deficiency results in resistance to hematopoietic growth factors (e.g. erythropoietin), and impairs the differentiation and maturation of all types of hematopoietic cells.15
Treatment of anemia in heart failureThere is no universally agreed definition of anemia. The World Health Organization considers anemia to exist when Hb levels are lower than 13 g/dl in men and 12 g/dl in women.20 Others define it as hematocrit less than 35–39%.21 The target Hb level in patients with anemia is also not agreed, but 12 g/dl is regarded as safe.22
The association of anemia with worse prognosis, functional capacity and quality of life in HF has prompted efforts to correct this comorbidity. Besides blood transfusion, which is recommended for severe anemia,23 there are two main types of treatment of anemia in HF: erythropoietic stimulating agents (ESAs) and iron supplementation.
Erythropoietic stimulating agentsErythropoietin, which is produced in the kidneys in response to hypoxia, acts on the bone marrow to promote the survival and proliferation of erythroid precursor cells, increasing the production of red blood cells. Recombinant human erythropoietin (rHuEPO) and a more recent erythropoietin analog with a longer half‐life, darbepoetin alfa, have been used in various trials to treat anemia associated with HF. The rationale for using ESAs is that although anemia in HF is multifactorial, it may represent an absolute or a relative deficiency or resistance to endogenous erythropoietin.
Silverberg et al. were the first to use ESAs in patients with anemia and HF, in an open randomized trial of 32 patients with moderate to severe HF and Hb 10–11.5 g/dl.24 Treatment with rHuEPO and intravenous (IV) iron was followed by improvement in NYHA class, increased left ventricular ejection fraction and reductions in hospitalizations and need for diuretics. Several small‐scale studies with rHuEPO or darbepoetin alfa have shown improvements in oxygen uptake and functional capacity, reduced BNP levels and improved quality of life.25–27 However, the results have been inconsistent. In a study by van Veldhuisen et al. of 165 patients with HF and Hb between 9.1 and 12.5 g/dl,28 administration of darbepoetin alfa for a target value of 14 g/dl raised Hb levels and improved some quality of life indices as assessed by the Kansas City Cardiomyopathy Questionnaire, but no improvements were seen in the 6‐minute walk test, NYHA functional class, or Minnesota Living with Heart Failure score.
A meta‐analysis published in 2011 of 11 randomized clinical trials, nine placebo‐controlled and five double‐blinded, of a total of 794 patients with HF and anemia treated with ESAs showed improvements in symptoms and functional capacity and a reduction in clinical events.29 It should be noted that in many of the small published trials iron supplementation was used in association with ESAs.
However, the latest evidence does not support the use of ESAs to treat anemia in HF. The lack of demonstrated benefit, and indeed the associated risks, were demonstrated in the Reduction of Events by Darbepoetin Alfa in Heart Failure (RED‐HF) trial, which randomized 2278 patients with systolic HF and anemia to receive darbepoetin alfa or placebo, with a target Hb level of 13.0 g/dl.30 Oral or IV iron was administered as tolerated if TSAT fell to less than 20% at any time. No significant differences were seen in the composite primary outcome of death from any cause or hospitalization for worsening heart failure in a mean follow‐up of 28 months (50.7% in the darbepoetin alfa group and 49.5% in the placebo group (hazard ratio 1.01; 95% confidence interval [CI] 0.90–1.13) or in the incidence of stroke, although the latter was slightly higher in the darbepoetin alfa group (3.7% vs. 2.7%). However, thromboembolic events were more frequent in the darbepoetin alfa group (13.5% vs. 10%).
These results are similar to those of the Trial to Reduce Cardiovascular Events with Aranesp Therapy (TREAT), which compared darbepoetin alfa with placebo in 4028 patients with diabetes, chronic kidney disease, and anemia, a third of whom had HF.31 Higher rates of stroke and thromboembolic events were seen in the darbepoetin alfa group.
Possible reasons for the adverse events seen with the use of ESAs include worsening of hypertension, elevated thromboembolic risk and increased release of endothelin.
Intravenous iron supplementationThe disappointing results reported for ESAs contrast with those described for IV iron supplementation alone in patients with HF and iron deficiency, even without manifest anemia.
The use of IV iron in the form of ferric carboxymaltose for the treatment of anemia of various causes was reviewed in a 2011 meta‐analysis of 11 randomized trials and three cohort studies.32 A total of 2348 patients were treated with IV ferric carboxymaltose in randomized trials and 348 in cohort studies, 832 receiving oral iron, 762 receiving placebo and 384 receiving IV iron sucrose. Compared to oral iron (the most common comparator), IV ferric carboxymaltose increased mean Hb by 4.8 g/dl, ferritin by 163 μg/l and TSAT by 5.3%, and was significantly better than comparator in achieving the target Hb level (number needed to treat: 5.9). The incidence of serious adverse events was similar with IV ferric carboxymaltose and comparator, but gastrointestinal adverse events were significantly more frequent in patients treated with oral iron.
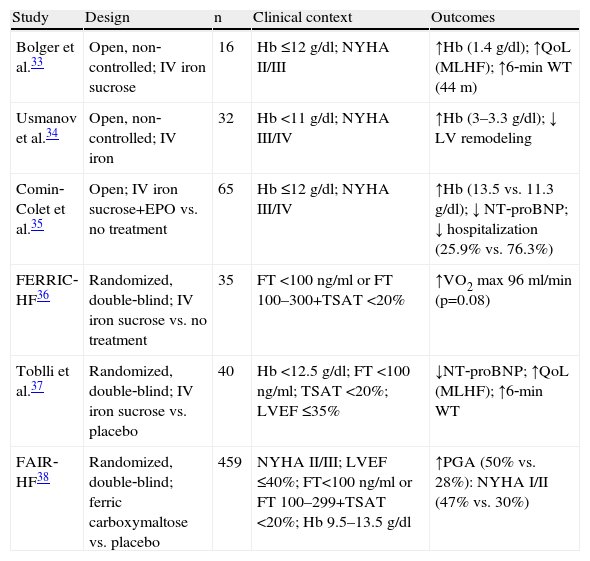
Six studies have been published on iron supplementation in HF, including two open non‐controlled trials,33,34 one open controlled trial,35 and three randomized placebo‐controlled, double‐blind trials36–38 (Table 2).
Studies on intravenous iron supplementation in patients with heart failure and anemia or iron deficiency.
| Study | Design | n | Clinical context | Outcomes |
| Bolger et al.33 | Open, non‐controlled; IV iron sucrose | 16 | Hb ≤12 g/dl; NYHA II/III | ↑Hb (1.4 g/dl); ↑QoL (MLHF); ↑6‐min WT (44 m) |
| Usmanov et al.34 | Open, non‐controlled; IV iron | 32 | Hb <11 g/dl; NYHA III/IV | ↑Hb (3–3.3 g/dl); ↓ LV remodeling |
| Comin‐Colet et al.35 | Open; IV iron sucrose+EPO vs. no treatment | 65 | Hb ≤12 g/dl; NYHA III/IV | ↑Hb (13.5 vs. 11.3 g/dl); ↓ NT‐proBNP; ↓ hospitalization (25.9% vs. 76.3%) |
| FERRIC‐HF36 | Randomized, double‐blind; IV iron sucrose vs. no treatment | 35 | FT <100 ng/ml or FT 100–300+TSAT <20% | ↑VO2 max 96 ml/min (p=0.08) |
| Toblli et al.37 | Randomized, double‐blind; IV iron sucrose vs. placebo | 40 | Hb <12.5 g/dl; FT <100 ng/ml; TSAT <20%; LVEF ≤35% | ↓NT‐proBNP; ↑QoL (MLHF); ↑6‐min WT |
| FAIR‐HF38 | Randomized, double‐blind; ferric carboxymaltose vs. placebo | 459 | NYHA II/III; LVEF ≤40%; FT<100 ng/ml or FT 100–299+TSAT <20%; Hb 9.5–13.5 g/dl | ↑PGA (50% vs. 28%): NYHA I/II (47% vs. 30%) |
EPO: erythropoietin; FT: ferritin; Hb: hemoglobin; IV: intravenous; LV; left ventricular; LVEF: left ventricular ejection fraction; MLHF: Minnesota Living with Heart Failure score; PGA: Patient Global Assessment score; QoL: quality of life; TSAT: transferrin saturation; VO2 max: peak oxygen uptake; 6‐min WT: 6‐minute walk test.
Improvements in symptoms, exercise capacity and quality of life were seen in parallel with rises in Hb levels in all these studies. In the Ferric Iron Sucrose in Heart Failure (FERRIC‐H) trial, symptoms and exercise capacity also improved, although to a lesser extent, in non‐anemic patients.36 Improved oxygen consumption did not relate to absolute increases in Hb but to increased TSAT.
The multicenter randomized double‐blind placebo‐controlled Ferinject Assessment in Patients with Iron Deficiency and Chronic Heart Failure (FAIR‐HF) trial was the largest.38 Treatment with ferric carboxymaltose significantly improved the two main outcomes: 50% of patients randomized to ferric carboxymaltose reported at least moderate improvement on the Patient Global Assessment questionnaire, compared to 28% of the placebo group (odds ratio [OR] for improvement 2.51, 95% CI 1.75–3.61), and 47% of the treatment group achieved NYHA class I or II, compared to 30% in the placebo group (OR 2.40, 95% CI 1.55–3.71). Improvements were also seen in the 6‐minute walk test and in quality of life scores, but prognosis was not affected (despite a tendency for fewer hospitalizations in the treatment group); the trial was not designed to assess the effect of iron supplementation on prognosis. The benefits of iron supplementation were seen in patients without as well as with anemia; this is slightly puzzling, but may be explained by the fact that only low‐intensity exercise was tested, which correlates with iron levels in tissues. If maximum aerobic capacity had been tested, the non‐anemic group would probably not have shown improvement, since this parameter depends on Hb concentrations rather than muscle oxidative capacity.39
The question arises as to whether similar results could be obtained with oral iron. Absorption of oral iron(II) is blocked by hepcidin; moreover, gastrointestinal tolerance of oral iron drugs is generally poor, and they interact with various other medications, including proton pump inhibitors.40 Furthermore, even if the iron is absorbed, its transport to the bone marrow is blocked by hepcidin, as in cases of anemia of chronic disease, which do not respond to oral iron. In IV formulations, iron in the form of iron(III) is bound to carbohydrate complexes, which are taken up from the bloodstream into the reticuloendothelial system within hours of administration. Most is incorporated into iron stores, but some binds to transferrin and reaches the bone marrow, thus overcoming blockade by hepcidin and resulting in underuse of this iron in tissue storage sites, formation of free radicals and increased risk of infection due to reduced cellular immunity and bacterial growth enhancement.41 However, the FAIR‐HF trial did not show higher rates of infection or cardiovascular events. Unlike the iron dextran previously used, current IV iron preparations such as iron sucrose, ferric gluconate and ferric carboxymaltose are well tolerated, rarely causing hypersensitive reactions, and thus do not require a test dose.42
A recent study shows improvements in previously low health‐related quality of life after four weeks of treatment with ferric carboxymaltose irrespective of previous anemia status.43
A health economic analysis of ferric carboxymaltose for HF patients with or without anemia in the UK showed the treatment to be cost‐effective, below the threshold of 22 200–33 300 euros per quality‐adjusted life year gained typically used by the UK National Institute for Health and Clinical Excellence, and robust in sensitivity.44
Three clinical trials are currently underway comparing ferric carboxymaltose with placebo in patients with HF and iron deficiency: CONFIRM‐HF (NCT01453608), with 300 patients, and iCHF (NCT01837082), with 100 patients, both ending in December 2013; and EFFECT‐HF (NCT01394562), with 160 patients, due to end in January 2014. These trials are intended to determine the efficacy of ferric carboxymaltose in terms of improving functional capacity, and its safety. A combined analysis of the results of FAIR‐HF and these trials will also show whether ferric carboxymaltose reduces clinical events such as death and hospitalization for HF.
Guidelines for heart failureThere are no specific recommendations for the management of patients with HF and anemia or iron deficiency in the American or European guidelines (the latter adopted by the Portuguese Society of Cardiology).45,46 There is a general recommendation in the European guidelines for the management of anemia: “A standard diagnostic work‐up should be undertaken in anemic patients. Correctable causes should be treated in the usual way.”45 It also states that IV ferric carboxymaltose may be considered for patients with iron deficiency.
Case studyAlthough not considered relevant at the initial assessment, the patient's Hb level of 11 g/dl will reduce her functional capacity and contribute to risk of morbidity and mortality. According to the European guidelines on HF, a diagnostic work‐up of her anemia should have been performed, as well as medical therapy and echocardiographic assessment. Serum ferritin <100 ng/ml or 100–299 ng/ml associated with TSAT <20% indicates inflammation or chronic disease as the cause and should be corrected by iron supplementation, preferably parenterally.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Gil VM, Ferreira JS. Anemia e deficiência de ferro na insuficiência cardíaca. Rev Port Cardiol. 2014;33:39–44.