Cardiac magnetic resonance (CMR) imaging is increasingly important in the diagnostic work-up of a wide range of heart diseases, including those with arrhythmogenic potential.
ObjectiveTo assess the added value of CMR in etiological diagnosis of ventricular arrhythmias after an inconclusive conventional investigation.
MethodsPatients undergoing CMR between 2005 and 2011 for investigation of ventricular arrhythmias were included (n=113). All had documented arrhythmias. Those with a definite diagnosis from a previous investigation and those with evidence of coronary artery disease (acute coronary syndrome, typical angina symptoms, increase in biomarkers or positive stress test) were excluded. CMR results were considered relevant when they fulfilled diagnostic criteria.
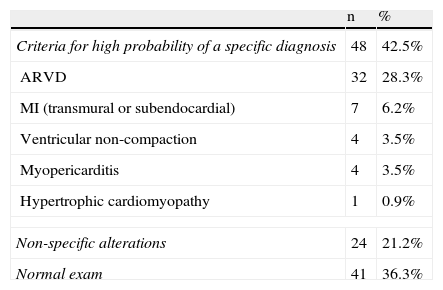
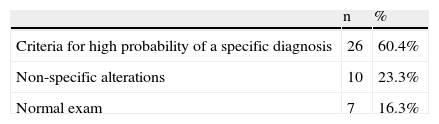
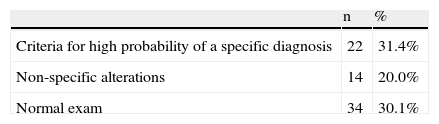
ResultsOf the 113 patients, 57.5% were male and mean age was 41.7±16.2 years. Regarding the initial arrhythmia, 38.1% had ventricular fibrillation/sustained ventricular tachycardia (VF/VT) and 61.9% had less complex ventricular ectopy. CMR imaging showed criteria of a specific diagnosis in 42.5% of patients, was totally normal in 36.3%, and showed non-specific alterations in the remainder. In VF/VT patients, specific criteria were found in 60.4%, and in 31.4% of those with less complex ectopy.
The most frequent diagnoses were arrhythmogenic right ventricular dysplasia, ventricular non-compaction and myopericarditis. It is worth noting that, although there was no evidence of previous coronary artery disease, 6.2% of patients had a late gadolinium enhancement distribution pattern compatible with myocardial infarction.
ConclusionCMR gives additional and important information in the diagnostic work-up of ventricular arrhythmias after an inconclusive initial investigation. The proportion of patients with diagnostic criteria was 42.5% (60.0% in those with VF/VT), and CMR was completely normal in 36.6%.
A ressonância magnética cardíaca (RMC) tem vindo a adquirir grande relevância na avaliação diagnóstica de um espectro cada vez mais amplo de cardiomiopatias, incluindo as que apresentam potencial arritmogénico.
ObjetivoAvaliação do valor acrescentado da RMC no diagnóstico etiológico de arritmias ventriculares, quando a investigação convencional inicial com outros métodos complementares de diagnóstico não é conclusiva.
MétodosEstudaram-se retrospetivamente os doentes que realizaram RMC para esclarecimento da etiologia de arritmias ventriculares, entre 2005-2011 (n = 113). Foram incluídos apenas doentes com arritmias ventriculares documentadas. Constituíram critérios de exclusão a obtenção de diagnóstico definitivo por exame complementar, de diagnóstico realizado previamente e a presença de história prévia sugestiva de doença coronária (antecedentes de síndrome coronária aguda ou história de angor típico, de elevação de biomarcadores de necrose miocárdica ou teste de isquemia positivo, quando realizado). Os resultados da RMC foram considerados relevantes quando sugeriram um diagnóstico provável.
ResultadosDos 113 doentes incluídos, 57,5% eram homens. A idade média foi 41,7 ± 16,2 anos. Quanto à arritmia documentada, 38,1% dos doentes foram referenciados por taquicardia ventricular/fibrilhação ventricular (FV/TV mantida) e 61,9% por extrassistolia ventricular com menor complexidade (ESV). A RMC mostrou alterações sugestivas de um diagnóstico específico em 42,5% dos doentes, foi totalmente normal em 36,3% e mostrou alterações inespecíficas nos restantes. Nos casos de referenciação por FV/TV mantida a RMC foi diagnóstica em 60,4% dos casos, enquanto nos casos de ESV foi-o em 31,4%.
Os diagnósticos prováveis mais frequentes foram displasia arritmogénica do ventrículo direito, não compactação ventricular e miopericardite. Assinala-se que, apesar da ausência de evidências clínicas sugestivas pelos critérios atrás referidos, 6,2% dos doentes apresentaram áreas de realce tardio com distribuição e características atribuíveis a doença coronária obstrutiva.
ConclusãoA RMC proporciona valor acrescentado no diagnóstico etiológico de arritmias ventriculares quando exames mais acessíveis ou realizados previamente não são conclusivos. A percentagem de doentes em que foi conclusiva foi de 42,5% (60,4% nos casos de referenciação por FV/TV mantida) e em que foi totalmente normal foi de 36,3%.
Cardiac magnetic resonance (CMR) imaging is a diagnostic technique that can characterize a wide range of pathophysiological phenomena, and can thus be considered a “broad-spectrum” exam. It is capable of accurately determining the morphological and functional characteristics of a variety of conditions, without the limitations of the acoustic windows and views of other imaging modalities and with excellent resolution; these advantages are particularly useful in assessing the right chambers. It can also characterize pathological processes that cause irreversible tissue damage (revealed by late gadolinium enhancement) and those in which tissue damage is recent or ongoing (by showing areas of ‘edema’ in T2-weighted images).1 The pattern and distribution of these changes can be used to identify the etiology of the pathological process with varying degrees of sensitivity and specificity.2,3 Moreover, the presence and distribution of adipose tissue can be detected in T1-weighted images, demonstrating fatty infiltration in the myocardium, as in arrhythmogenic cardiomyopathy.4,5
Current guidelines recommend that the diagnostic work-up of ventricular arrhythmias should exclude structural heart disease (by echocardiography) and coronary artery disease (CAD),6,7 further diagnostic exams being at the discretion of the attending physician.8
Bearing in mind the wide range of pathophysiological processes and mechanisms that can trigger ventricular arrhythmias, and the ability of CMR to detect the characteristic features that indicate a higher probability of a particular disorder, there is a sound theoretical foundation for the use of CMR in the investigation of the underlying etiology of ventricular arrhythmias in situations in which initial exams fail to provide a conclusive diagnosis.
ObjectiveThe aim of this study was to ass the value of CMR in etiological diagnosis of ventricular arrhythmias when the initial diagnostic exams requested by the attending physician in accordance with standard practice are inconclusive.
MethodsPatients referred to a reference center for CMR between 2005 and 2011 for etiological investigation of ventricular arrhythmias, following inconclusive initial conventional exams requested by the attending physician in accordance with standard practice, were enrolled retrospectively. All had undergone transthoracic echocardiography, and those with intermediate risk of CAD (on the basis of age, gender and symptoms) had undergone testing for ischemia. Patients were included whose ventricular arrhythmias were considered by the referring physicians (cardiologists in all cases) to require investigation by CMR of an arrhythmogenic substrate, due to their complexity, frequency, morphology or clinical repercussions. Patients with a history suggestive of CAD (previous acute coronary syndrome, typical angina symptoms, increase in biomarkers or positive stress test) were excluded.
The diagnoses of myocarditis, hypertrophic cardiomyopathy, arrhythmogenic cardiomyopathy and ventricular non-compaction were based on the criteria in the respective guidelines,9–13 while a diagnosis of CAD was made when late enhancement was observed subendocardially in locations consistent with the distribution of the coronary arteries.
Morphological and functional studies were performed in all patients using a 1.5 T Siemens Magnetom Symphony Maestro Class scanner, obtaining T1- and T2-weighted and late enhancement images.
Functional assessment was by steady-state free precession (SSFP) sequences (TE 1.5 ms; TR 43.26 ms; slice thickness 6 mm; flip angle 80°; matrix 192 × 192) with the cardiac cycle divided into 30-mm segments.
Morphological assessment was based on T1-weighted (TE 7.5 ms; TR 700 ms; slice thickness 6 mm; flip angle 180°; matrix 256 × 125) and T2-weighted (TE 46 ms; TR 800 ms; slice thickness 5 mm; flip angle 180°; matrix 256 × 157) turbo spin echo sequences.
Late enhancement images were obtained 10 min after the administration of 0.2 mmol/kg of intravenous contrast (gadolinium chelate), using phase-sensitive inversion recovery (PSIR) (TE 1.44 ms; TR 250 ms; slice thickness 8 mm; flip angle 45°; matrix 256 × 167).
After processing, the images were interpreted jointly by a cardiologist and a radiologist, who decided whether a particular disease was likely to be present based on the imaging results, clinical data provided by the referring physician and the diagnostic criteria, or whether the findings were normal or non-specific.
ResultsA total of 113 patients were analyzed, mean age 41.7±16.2 years.
DiscussionIn the most recent (2006) American and European guidelines for management of patients with ventricular arrhythmias,6 echocardiography and non-invasive methods for detecting myocardial ischemia (exercise testing, myocardial perfusion scintigraphy and pharmacological stress echocardiography) are class I recommendations for investigation of arrhythmic substrates. CMR is indicated when echocardiography does not provide accurate information on functional and structural changes in both ventricles (class IIa recommendation, level of evidence B), while coronary angiography should be considered in patients with life-threatening ventricular arrhythmias or in survivors of sudden cardiac death, who have an intermediate or higher pretest probability of having CAD based on age, symptoms, and gender (class IIa recommendation, level of evidence C).
Even when conventional echocardiography provides a complete assessment of structural and functional alterations in both ventricles, as referred to in the guidelines, it cannot attribute these changes to a specific underlying pathophysiological process, since echocardiography is incapable of characterizing tissue abnormalities. For example, left ventricular wall motion abnormalities, even when located in a specific arterial territory, may be due to a local inflammatory process of a different etiology, and not to ischemia. The guidelines did not assign a class of recommendation to myocardial perfusion CMR in the diagnosis of significant CAD or silent ischemia, but in 2006 they acknowledged that its cost and availability were becoming more competitive; it is thus clear that certain advantages of CMR make it more useful in this context than was recognized in the 2006 guidelines.
In recent years, the situation has changed; CMR is increasingly seen as having an important role in diagnostic investigation when there is suspicion of heart disease with arrhythmogenic potential, of which the following are examples:
Hypertrophic cardiomyopathy: In the latest guidelines for the diagnosis and treatment of hypertrophic cardiomyopathy,11 CMR is assigned a class I recommendation in patients in whom echocardiography is suggestive but not conclusive, or when additional information is required that may affect decision-making, such as assessment of hypertrophied segments, the presence of aneurysms, or the anatomy of the mitral valve apparatus. CMR may also be considered to aid differential diagnosis with amyloidosis, Fabry disease and LAMP2 cardiomyopathy, and late enhancement study is useful for prognostic and arrhythmic risk stratification.
Myocarditis: Given the degree of synergy between CMR findings and endomyocardial biopsy,14 CMR is currently considered a first-line exam for patients with suspected myocarditis or non-ischemic cardiomyopathy.15 Although its disadvantages are also recognized, particularly its inability to diagnose special forms of myocarditis such as giant cell or eosinophilic myocarditis, which require specific therapies, CMR can help determine long-term prognosis and stratify risk of potentially fatal events, including ventricular arrhythmias.16
Arrhythmogenic right ventricular dysplasia/arrhythmogenic cardiomyopathy: The superior ability of CMR to assess the dimensions and function of the right ventricle was recognized in the 2010 revision of the diagnostic criteria for arrhythmogenic right ventricular dysplasia/arrhythmogenic cardiomyopathy,12 with CMR reference values being incorporated into the criteria, unlike the original criteria published in 1994, which were based on symptomatic index cases with relatively advanced disease and were thus less sensitive for detection of early stages of the disease.17 However, histological demonstration of fibrofatty accumulation at biopsy remains necessary, and CMR T1-weighted images are still considered non-specific.18
Ischemic heart disease: Besides the ability of CMR to detect fibrotic tissue, to diagnose obstructive CAD through perfusion studies and to assess myocardial viability by determining the extent of transmurality of the fibrotic area, there is increasing evidence that the characteristics of scar tissue, particularly transmurality, can help predict arrhythmic risk.19,20
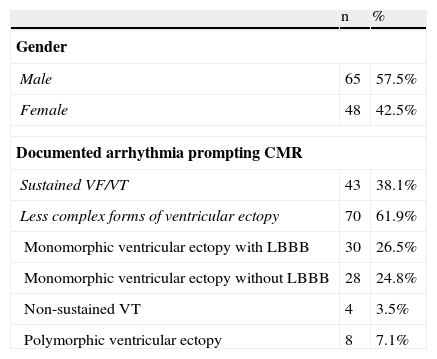
The ventricular arrhythmias requiring etiological investigation in our series included a variety of different forms of manifestation and prognosis, from frequent isolated ventricular ectopy to malignant forms degenerating to cardiopulmonary arrest (Table 1).
Baseline characteristics of the study population.
| n | % | |
| Gender | ||
| Male | 65 | 57.5% |
| Female | 48 | 42.5% |
| Documented arrhythmia prompting CMR | ||
| Sustained VF/VT | 43 | 38.1% |
| Less complex forms of ventricular ectopy | 70 | 61.9% |
| Monomorphic ventricular ectopy with LBBB | 30 | 26.5% |
| Monomorphic ventricular ectopy without LBBB | 28 | 24.8% |
| Non-sustained VT | 4 | 3.5% |
| Polymorphic ventricular ectopy | 8 | 7.1% |
CMR: cardiac magnetic resonance imaging; LBBB: left bundle branch block; VF/VT: ventricular fibrillation/sustained ventricular tachycardia; VT: ventricular tachycardia.
Our results confirm that in a significant number of cases CMR adds important information to conventional investigation of the pathological process underlying ventricular arrhythmias. The use of CMR on top of the conventional exams requested by the attending physician determined a specific cause in 42.5% of patients who had not been diagnosed. Furthermore, CMR was normal in 36.3% of cases, enabling diseases that would be considered in differential diagnosis to be excluded with a high degree of probability (Tables 2–4). CMR thus provided added diagnostic value in 78.8% of cases after the initial investigation. In the remaining 21.2%, the results, although not normal, did not indicate a specific cause, but provided additional information which, taken together with other findings, could help to exclude conditions that may have been suspected before the exam.
Overall contribution of cardiac magnetic resonance to diagnosis.
| n | % | |
| Criteria for high probability of a specific diagnosis | 48 | 42.5% |
| ARVD | 32 | 28.3% |
| MI (transmural or subendocardial) | 7 | 6.2% |
| Ventricular non-compaction | 4 | 3.5% |
| Myopericarditis | 4 | 3.5% |
| Hypertrophic cardiomyopathy | 1 | 0.9% |
| Non-specific alterations | 24 | 21.2% |
| Normal exam | 41 | 36.3% |
ARVD: arrhythmogenic right ventricular dysplasia; MI: myocardial infarction.
In patients referred for CMR due to arrhythmias known to carry a worse prognosis (ventricular fibrillation and sustained ventricular tachycardia), the percentage of CMR exams that fulfilled diagnostic criteria was even higher (60.4%), which highlights the value of this technique (Table 3).
Diagnoses: The diagnoses obtained in this study are generally in agreement with those of a study of the victims of sudden cardiac death, in whom autopsy studies revealed the most frequent causes of death to be myocarditis, arrhythmogenic right ventricular dysplasia, myocardial fibrosis associated with obstructive CAD and hypertrophic cardiomyopathy.21
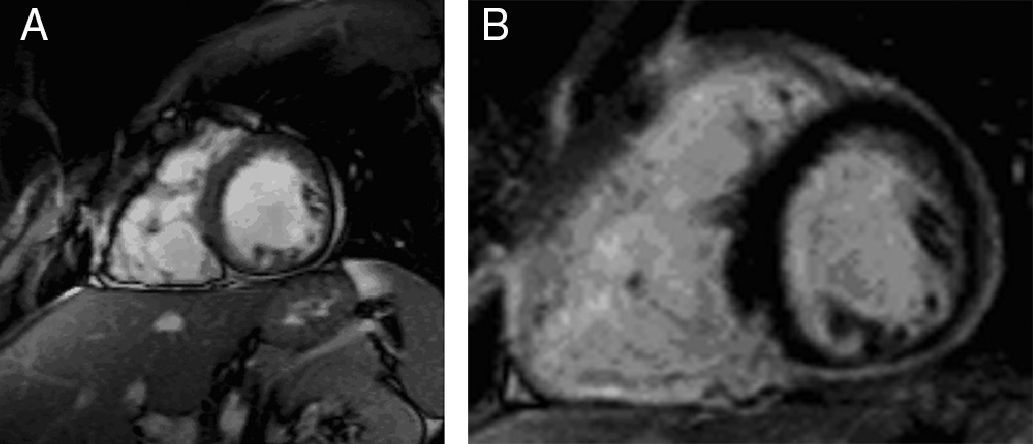
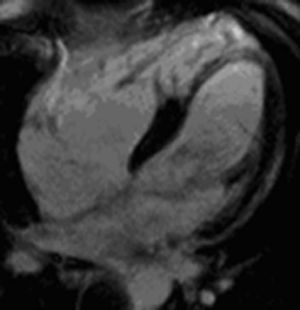
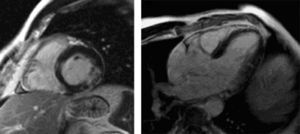
In our series, the most common trigger of ventricular arrhythmias was arrhythmogenic right ventricular dysplasia, criteria for which were found with a high probability in over a quarter of patients (Figures 1 and 2). This is partly explained by the high prevalence of arrhythmias with characteristics indicating an origin in the right ventricle; moreover, CMR is a first-line exam for diagnosing this disease, due to its high sensitivity for detecting fatty tissue through a hyperintense signal in T1-weighted images and its ability to provide a detailed assessment of the morphology and function of the right chambers – more so than in other entities with arrhythmogenic potential, in which other modalities can provide sufficient information, such as myocardial perfusion scintigraphy and coronary angiography in ischemic heart disease.
Pseudoaneurysms of the right ventricular free wall in short-axis view. (A) Steady-state free precession sequence; (B) phase-sensitive inversion recovery sequence. Late enhancement of the inferior septum and inferior wall of both ventricles, showing arrhythmogenic right ventricular dysplasia.
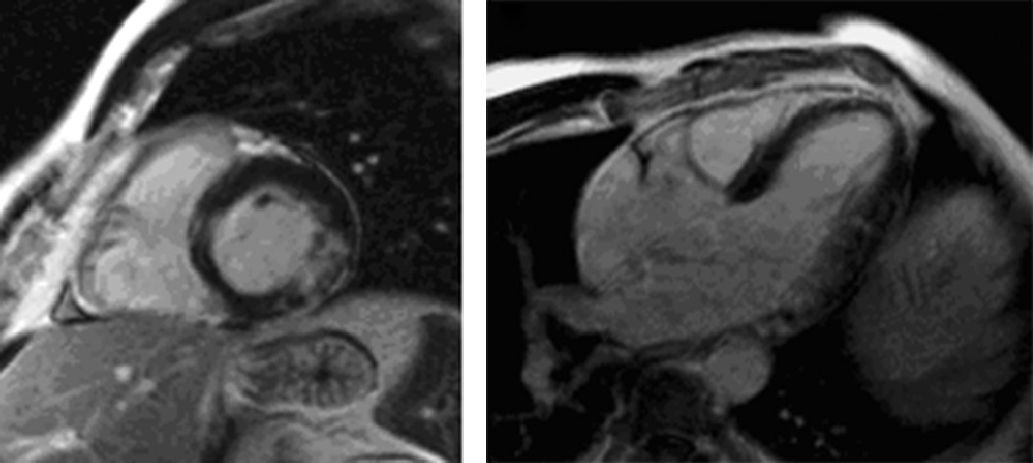
The prevalence of ischemic heart disease (6.2%) (Figure 3) in patients without a history of angina or known previous coronary events should be noted, highlighting the fact that silent ischemia can be responsible for the development of arrhythmogenic substrates, and the need to use diagnostic methods that test for myocardial ischemia when investigating arrhythmias of unknown etiology, as recommended in the guidelines.6
As the number of centers in which CMR is available increases, and as the medical community becomes more aware of its potential, it is likely that the number of referrals will rise and that it will be introduced at an earlier stage in the diagnostic algorithm to investigate the arrhythmogenic mechanism underlying ventricular ectopy.
There is now general recognition of the advantages of CMR, which in a single exam can provide structural and functional information, as well as assessing tissue composition, perfusion and myocardial viability.
LimitationsCertain limitations of this analysis should be noted. The study was retrospective and there was no follow-up or assessment of the impact of the information obtained on therapeutic decisions or of clinical events. Since this was a single-center study, investigation prior to CMR reflects current practices at the center, which may differ from those at other centers, possibly leading to bias.
The patients referred for CMR were selected by the attending cardiologists, and although the criteria used and the characteristics of the arrhythmias that prompted referral were based on best current practice, it would be impossible to avoid a certain degree of subjectivity in selection.
For logistical reasons, CMR was not performed at the time when the arrhythmias were documented, which may have affected the sensitivity of detection of T2-weighted images to detect edema, which may in turn have reduced the diagnostic effectiveness of the studies.
ConclusionsIn this analysis, CMR was shown to have good diagnostic performance after an initial inconclusive investigation with other diagnostic exams in accordance with current practice. This imaging modality can visualize phenotypical findings that are characteristic of or highly likely to be associated with a wide range of conditions, and can thus be considered a “broad-spectrum” exam. The results of our study demonstrate the role of CMR in etiological investigation of ventricular arrhythmias and highlight the importance of its use at an early stage of the diagnostic work-up; it should always be considered when the initial investigation proves inconclusive.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Cabanelas N, Vidigal Ferreira MJ, Donato P, et al. A ressonância magnética cardíaca como uma mais-valia no diagnóstico etiológico de arritmias ventriculares. Rev Port Cardiol. 2013;32:785–791.